Quick take: Three weeks, three truths: you’re already working with addiction, intake illusions hurt care, and silence is data. This SUD screening playbook puts it all together—one streamlined process that works whether clients disclose freely, stay quiet, or fall somewhere between.
Missed the series? Read Blog 1: The Hidden Truth, Blog 2: The Intake Illusion, and Blog 3: When Silence Speaks.
What We’ve Learned About SUD Screening (And Why It Matters)
Over three weeks, we’ve dismantled the myths that keep SUD screening inconsistent:
- First, if you work with people, you work with addiction—whether you ask or not
- Second, “intake illusions” create blind spots that derail treatment plans
- Finally, silence isn’t “no”—it’s information about safety, shame, or prior bad experiences
Even with these insights, many clinicians still approach substance use questions case-by-case, reading the room, waiting for the “right moment.” However, universal SUD screening isn’t about catching people. It’s about seeing the whole case so your plan actually works.
This SUD screening playbook gives you one consistent process that adapts to every client while maintaining the same professional standard you’d use for any other health screening.
The 5-Minute Universal SUD Screening (Your New Standard)
For every client, every time. Here’s your template:
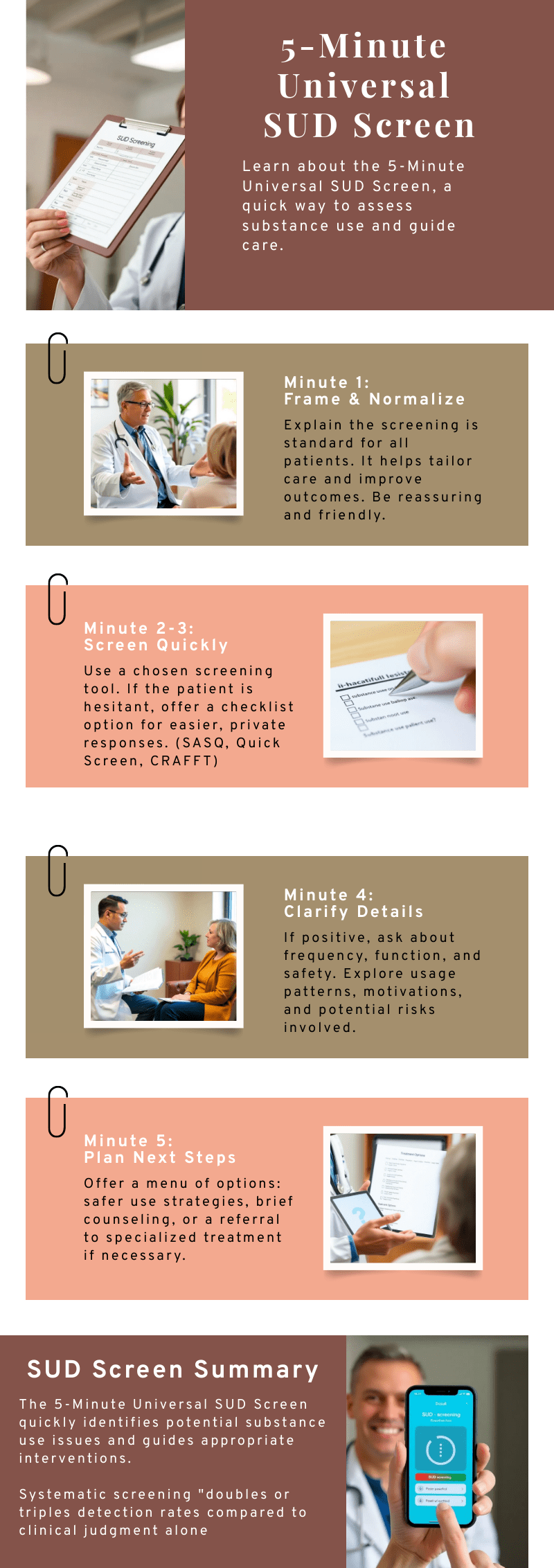
Minute 1: Frame & Normalize
“I ask everyone a few standard questions about alcohol, cannabis, and medications so I can tailor care appropriately. This helps me do a better job for you.”
Why this works: Sets expectation that everyone gets asked—reduces shame and personalizes care rather than targeting.
Minutes 2-3: SUD screening (Pick Your Tool)
Fortunately, validated screening tools like SASQ, CRAFFT, and NIDA Quick Screen provides clinical and legal protection by demonstrating adherence to evidence-based standards of care. Consistent documentation of screening completion shows due diligence in comprehensive assessment.
Adults – Alcohol Focus:
NIAAA SASQ: “How many times in the past year did you have 4+ (women)/5+ (men) drinks in a day?” If ≥1, expand with frequency/pattern questions
Adults – Multi-Substance:
NIDA Quick Screen: “In the past year, how often have you used an illegal drug or used a prescription for non-medical reasons?” If any use → TAPS for risk stratification
Adolescents:
CRAFFT 2.1 (self-administered version works well)
Additionally, when clients go quiet: Offer bridge: “Some people prefer a quick checklist they can hand back. What feels easier for you?”
Minutes 4-5: Clarify & Plan
Meanwhile, if any substance use is reported:
- Frequency: “What does a typical week look like?”
- Function: “What do you hope it helps with?”
- Safety: Any mixing with meds, driving, withdrawal concerns?
- Next step: Menu options (safer use, brief counseling, referral)
Documentation line: “Brief SUD screening completed ([tool used]). Client reports [frequency/pattern]. Discussed [safety concerns]. Plan: [specific next step]. Follow-up [when].”
SUD Screening Response System
Once you’ve completed the initial SUD screening, here’s how to handle each type of response:
Type 1: Open Disclosure
“I ask everyone a few quick questions about alcohol, cannabis, and medications so I can match care. Okay to do that now?”
Your response:
- Reflect back what you heard
- Scale motivation: “On 0-10, how important is it to keep use from interfering with your goals?”
- Link to treatment goals: “You mentioned sleep/anxiety/work stress—how does [substance] help with that, and how does it complicate it?”
- Offer immediate support: harm reduction tips, cravings plan, or brief counseling
Type 2: Uncertain/Minimizing
“Not really,” “sometimes,” “just weekends”
Your response:
- Normalize: “When you say ‘not really,’ help me understand what that looks like in a typical week”
- Specify: “Any days it’s more than you planned or interferes with sleep/work/relationships?”
- Validate: “A lot of people find themselves using more during stress—what’s been true for you?”
Type 3: Silent/Resistant
Long pauses, topic changes, “I’d rather not say”
Your response:
- Respect boundaries: “That’s okay. Would you prefer a private checklist you can hand back?”
- Offer options: “We can mark ‘prefer not to discuss’ and revisit later, or you can choose a yes/no format”
- Stay connected: “Either way, I want you to know this is a safe space to talk about anything affecting your health”
Quick Reference Cards (Keep These Handy)
Red Flag Combinations
Watch for silence + any of these:
- Sedative/stimulant prescriptions with vague injuries
- Monday absences, unexplained night sweats
- Respiratory issues with “anxiety” explanations
- Memory gaps during stressful periods
Action: Complete full validated SUD screening + safety planning

Emergency Bridges (When Clients Shut Down)
- Long pause:“Take your time. Many people use more than they intend. What’s been true for you?”
- Topic pivot:“We’ll get to scheduling. One quick question first about [substance]…”
- “Not really”:“When you say ‘not really,’ what does that look like—once a week, twice, not at all?”
- “I don’t want to answer”:“Totally fine. Want to tick a private checklist or should I mark ‘prefer not to discuss’?”
30-Second Safety Check
If any substance use reported:
- “Any mixing with prescribed medications?”
- “Any driving or operating equipment while using?”
- “Anyone to call if you need support reducing use?”
- “Any withdrawal symptoms when you stop?”

Common SUD Screening Pitfalls (And Quick Fixes)
As you implement this system, watch for these common pitfalls:
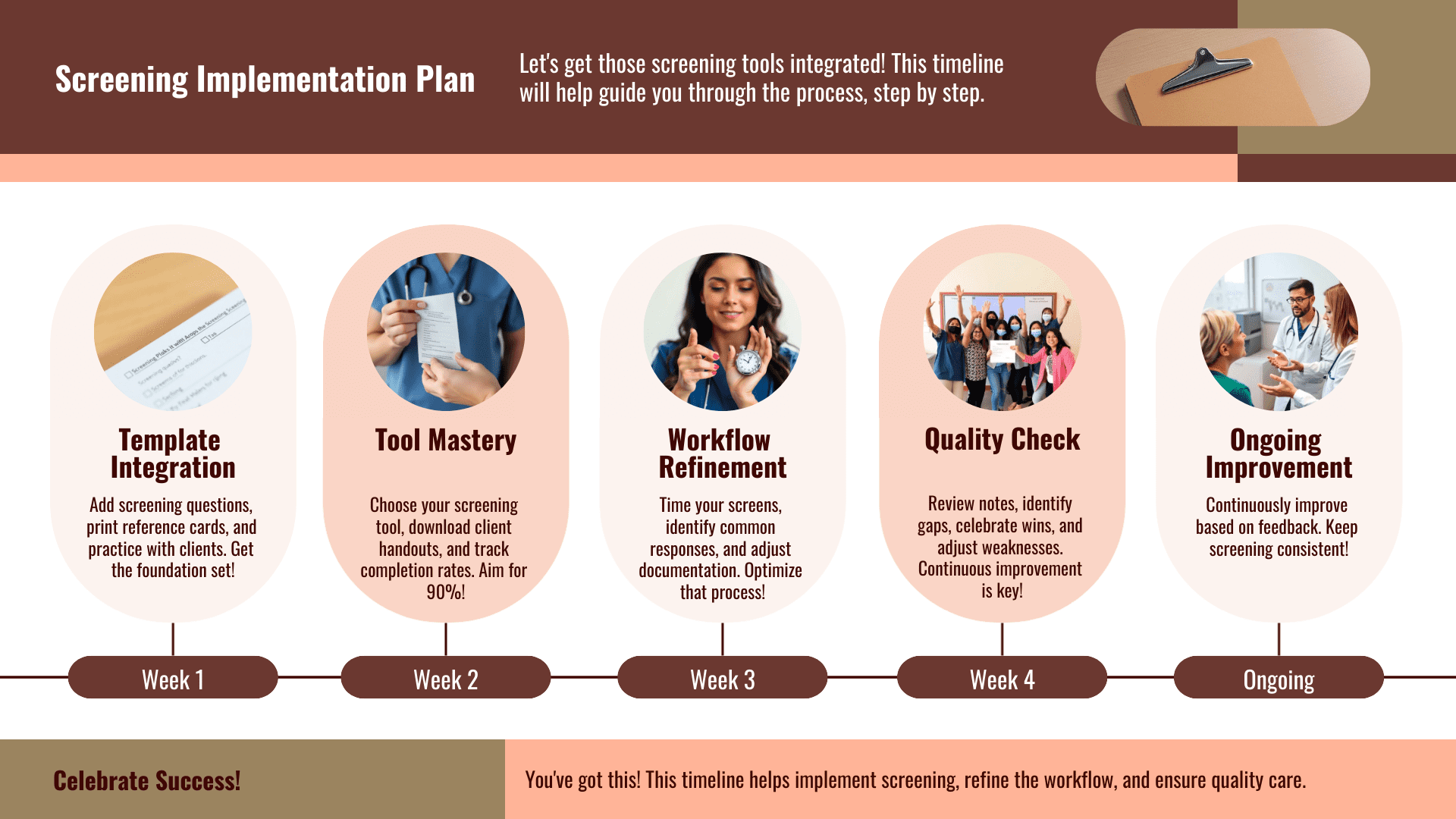
Pitfall: “I forgot to ask again”
Fix: Put SUD screening questions at the top of your intake template, not buried in the middle
Pitfall: “It feels awkward”
Fix: Practice the normalizing language until it sounds natural—most awkwardness comes from uncertainty, not content
Pitfall: “I don’t know what to do when they say yes”
Fix: Start with harm reduction basics (don’t mix with benzos, have a ride plan) while you build brief intervention skills
Pitfall: “My documentation is inconsistent”
Fix: Use the copy-paste template until you develop your own shorthand
Your Complete SUD Screening Resource Toolkit
To support your implementation, here’s your complete resource toolkit:
Start here – For clinicians conducting screening:
- Conversation Starter Guide (Interactive walkthrough for the complete SUD screening process – use this first)
Client resources – For positive screens or signs of problematic use:
- Safer Use Basics (Harm reduction – alcohol & cannabis)
- Cravings Plan 3-3-3 (Crisis planning tool)
- Medication Safety (Interaction warnings, storage guidance)
Clinical reference – For deeper implementation:
- NIAAA Core Resource (Alcohol screening & brief intervention)
- NIDA NMAssist (Multi-substance screening tools)
- SAMHSA SBIRT (Complete screening framework)
- FindTreatment.gov (Referral database)
Consistent screening (90%+ of intakes include substance use questions) → Client comfort (feedback indicates feeling heard, not judged)
Improved outcomes (better engagement when co-occurring issues addressed) → Clinical confidence (comfortable with brief interventions)
Why This Matters (One More Time)
Now that you have the complete system, let’s revisit why this work matters. Three weeks ago, I asked you to consider whether you might already be working with addiction without knowing it. If you’ve been following along, you now have:
- Language that normalizes rather than stigmatizes
- Tools that adapt to client comfort levels
- Brief interventions you can do in any setting
- Documentation that protects you and your clients
- Resources you can share immediately
But here’s what really matters: Every time you complete a thorough SUD screening, you’re not just checking a box. You’re seeing the whole person. You’re designing treatment that addresses what’s actually happening rather than what appears to be happening.
The clients who need this most are often the ones who seem to need it least. These include high-functioning professionals and trauma survivors. The chronic pain patient who takes “a few extra” pills on bad days.
Therefore, without asking, you’ll miss them. With consistent, compassionate SUD screening, you’ll catch them early—when brief interventions work best and before crises demand intensive care.
The Choice Is Yours
Four weeks ago, we started with a simple premise: if you work with people, you already work with addiction. Today, you have the tools to work with it intentionally.
You now have everything you need:
- A 5-minute SUD screening process that adapts to any client
- Language that opens doors instead of closing them
- Implementation steps that fit into your existing workflow
- Evidence-based tools that catch what intuition misses
But tools don’t change practice—clinicians do.
The difference between a missed opportunity and early intervention often comes down to five minutes and the courage to ask. The high-functioning attorney drinking herself to sleep. The veteran using cannabis for nightmares he won’t name. The teenager whose “anxiety” masks daily substance use.
They’re already in your caseload. The question isn’t whether you’ll encounter them—it’s whether you’ll see them.
Your next intake is an opportunity. Use it.
Therefore, without asking, you’ll miss them. However, with consistent, compassionate screening, you’ll catch them early…Ready to stop missing what matters? Download the complete campaign guide next week and transform your practice—one conversation at a time.
Share your commitment: Which screening tool are you implementing first? Comment below and join clinicians across the country who are choosing to see the whole person, not just the presenting problem.