Quick take: If your intake skips SUD Screening, you’re not protecting rapport—you’re protecting an illusion. A few neutral questions can change the entire course of care.
Missed Blog #1? Read The Hidden Truth — You’re Already Working with Addiction.
You don’t need a 60-minute evaluation to spot what matters—you need consistent SUD screening.
After last week’s post (“You’re already working with addiction”), this one zooms in on a common trap I see in intakes: we tell ourselves a compassionate story—they came for anxiety, there were no red flags, I didn’t want to hurt rapport—and that story quietly becomes permission to skip substance use questions. That’s the intake illusion.
Universal, brief SUD screening isn’t about catching people. It’s about seeing the whole case so your plan actually works. Thirty seconds of normalized questions (SBIRT-style) can change your differential, your risk assessment, and your next step—without derailing rapport.
In this post, I’ll name the most common “intake illusions,” offer reality checks, and give you swap-in micro-scripts, a 3-minute SUD screening flow, a one-line documentation template, and quick first-session interventions. There’s also a printable mini-poster to keep by your intake notes.
If you work with people, you already work with addiction. Let’s make sure your SUD screening shows it.
What I Hear in Intakes about SUD screening (and Why It Matters)





These sound reasonable in the moment. However, they can harden into habits that keep us from asking the most consequential questions in the room. When we don’t ask, we miss risk, misattribute symptoms, and design plans that fight an invisible current. This isn’t about catching people; it’s about seeing the whole case.
The 10 “Intake Illusions” about SUD screening (and what to say instead)
Each item includes (1) the illusion, (2) the reality check, and (3) a swap-in micro-script you can use today in your SUD screenings.
Documentation & liability myths
- Documentation will hurt them.”
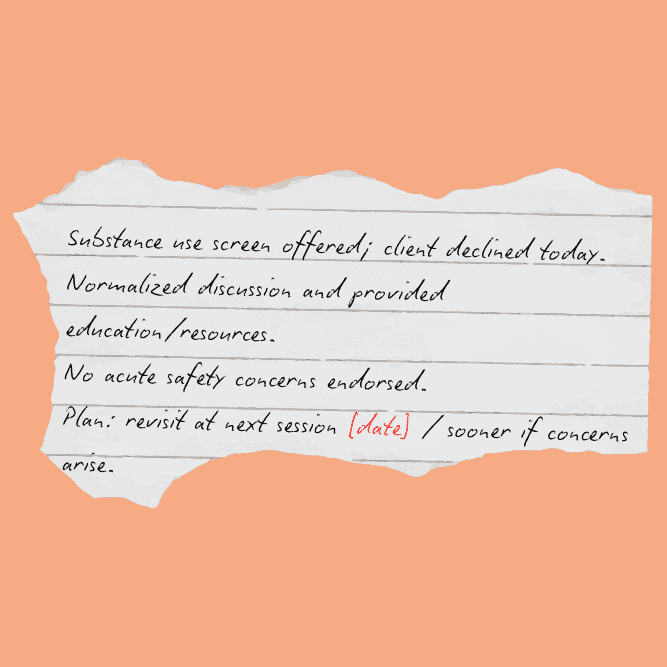
- Say (note line): “Client completed brief SUD screen; reports [frequency/type]; discussed risks/next steps; client consented to ongoing monitoring.”
- Reality: Ethical, factual notes protect clients and you.
Disclosure & rapport myths
- They’ll tell me if it’s a problem.”
- Reality: Most clients don’t disclose unprompted—shame and uncertainty are powerful silencers.
- Say:“I ask everyone a few standard questions about alcohol, cannabis, prescriptions, and other substances so I can tailor care. What does a typical week look like for you?”
- (Why standardize? See SAMHSA’s SBIRT overview.)
- No red flags.”
- Reality: Absence of visible risk ≠ absence of use. Many patterns look “high-functioning.”
- Say:“In the past 3 months, how often have you had 4/5+ drinks in a day? Used cannabis? Taken any extra pills or meds not as prescribed?”
- (Alcohol screen options: AUDIT-C; USPSTF recommends adult alcohol screening in primary care—see the Unhealthy Alcohol Use recommendation at USPSTF.)
- “I didn’t want to hurt rapport.”
- Reality: Clients feel safer when you normalize and ask the same of everyone.
- Say: “I ask these questions with every client—some people use, some don’t. Your answers help me do a better job.”
Scope & “not my job” assumptions
- “The presenting problem isn’t addiction.”
- Reality: Use can drive sleep, mood, pain, trauma responses, and treatment adherence.
- Say: “Because substances can affect anxiety/trauma/sleep, I want to check in on them briefly so we don’t miss anything.”
- (For alcohol-specific coaching language, see NIAAA’s Clinician’s Core Resource.)
- “The PCP/psychiatrist covers that.”
- Reality: Division of labor is not duplication of care. Screens are quick and collaborative.
- Say: “I’ll do a brief screen here and share themes with your prescriber so we’re aligned.”
- (Drug screens & brief interventions: NIDA Quick Screen & TAPS.)
Time & workflow constraints
- “We ran out of time.”
- Reality: A validated single-item screen takes under 30 seconds.
- Say: “Before we wrap: how many times in the past year have you used an illegal drug or used a prescription for non-medical reasons?”
- If ≥1: “Thanks for telling me. Let’s set time next session to dig in.”
- (More options when you do have time: WHO ASSIST. For adolescents, use CRAFFT 2.1.)
Tests vs. talking
- “The tox screen will tell me.”
- Reality: Labs are snapshots. Screens capture patterns, intent, and function.
- Say: “Regardless of labs, I ask about typical frequency, reasons for use, and any ‘more than intended’ moments.”
Recovery status blind spots
- “They’re in recovery, so we’re good.”
- Reality: Recovery status is dynamic. Screens are respect, not suspicion.
- Say: “What supports your recovery right now? Any recent close calls or increases in cravings?”
- “I can tell by looking.”
- Reality: Bias. You can’t.
- Say: “I use the same 4 questions with everyone; it keeps me thorough and fair.”
A 3-Minute SUD Screening That Actually Works
- Normalize – “I ask everyone about substances—some use, some don’t.”
- Screen (pick one):
- Single-Item (drug non-medical use in past year) via NIDA Quick Screen
- Alcohol: AUDIT-C (USPSTF supports adult alcohol screening: details)
- Broader: WHO ASSIST; Adolescents: CRAFFT 2.1
- (see Conversation Starter Guide for scripts)
- Clarify – frequency, amount, route, mixing with meds, “more than intended.”
- Function – “What do you hope the substance does for you?”
- Safety & Next Step – meds interactions, driving, withdrawal risk; schedule a focused visit or warm handoff.
When It’s Positive: First-Session Interventions (5 minutes or less)
- First reflect & scale. “On a 0–10, how important is it to keep use from getting in the way of your goals? What makes it that number and not lower?”
- Next link to goals. “You said sleep/parenting/work matters most—how does alcohol/cannabis help and how does it complicate that?”
- Then, offer a menu of next steps. 1) brief counseling here, 2) recovery supports, 3) medical consult (med interactions, withdrawal), 4) specialty SUD referral via FindTreatment.gov.
- Meanwhile, add quick harm-reduction tips. Don’t mix with benzos/opioids (see FDA boxed-warning communication: FDA drug safety & availability); avoid driving; avoid using alone; set a quantity/$$ cap; carry naloxone where relevant (CDC naloxone guidance).
- If cannabis is part of the picture, share a neutral overview from the CDC on cannabis health effects.
Common Pitfalls & Tiny Fixes
- Forms ask; clinicians connect. Say it out loud when the EHR has the question—forms don’t build trust.
- Yes/no boxes → open questions. Pivot to specific: “What does a typical week look like?”
- Rapport follows consistency. Ask early, then revisit gently.
- Risk over story. Capture the essentials: frequency, amount, route, risks, and plan.
Copy-Paste: Four Neutral Intake Questions for SUD Screening
To make the ask effortless, keep these on your template:
- “In the last 3 months, what does a typical week of alcohol look like for you?”
- “Any cannabis or CBD products? How often and in what form?”
- “Have you taken any prescriptions more than directed or anyone else’s medication?”
- “Any other substances, even rarely—cocaine, meth, club drugs, pills, or powders?”
If the client says yes to anything, follow with: “Tell me about the part you like and the part that’s not working? What would you be open to changing first? When do you find it most helpful—and when does it get in the way?”

Need ready-to-use language? Grab the Conversation Starter Guide.
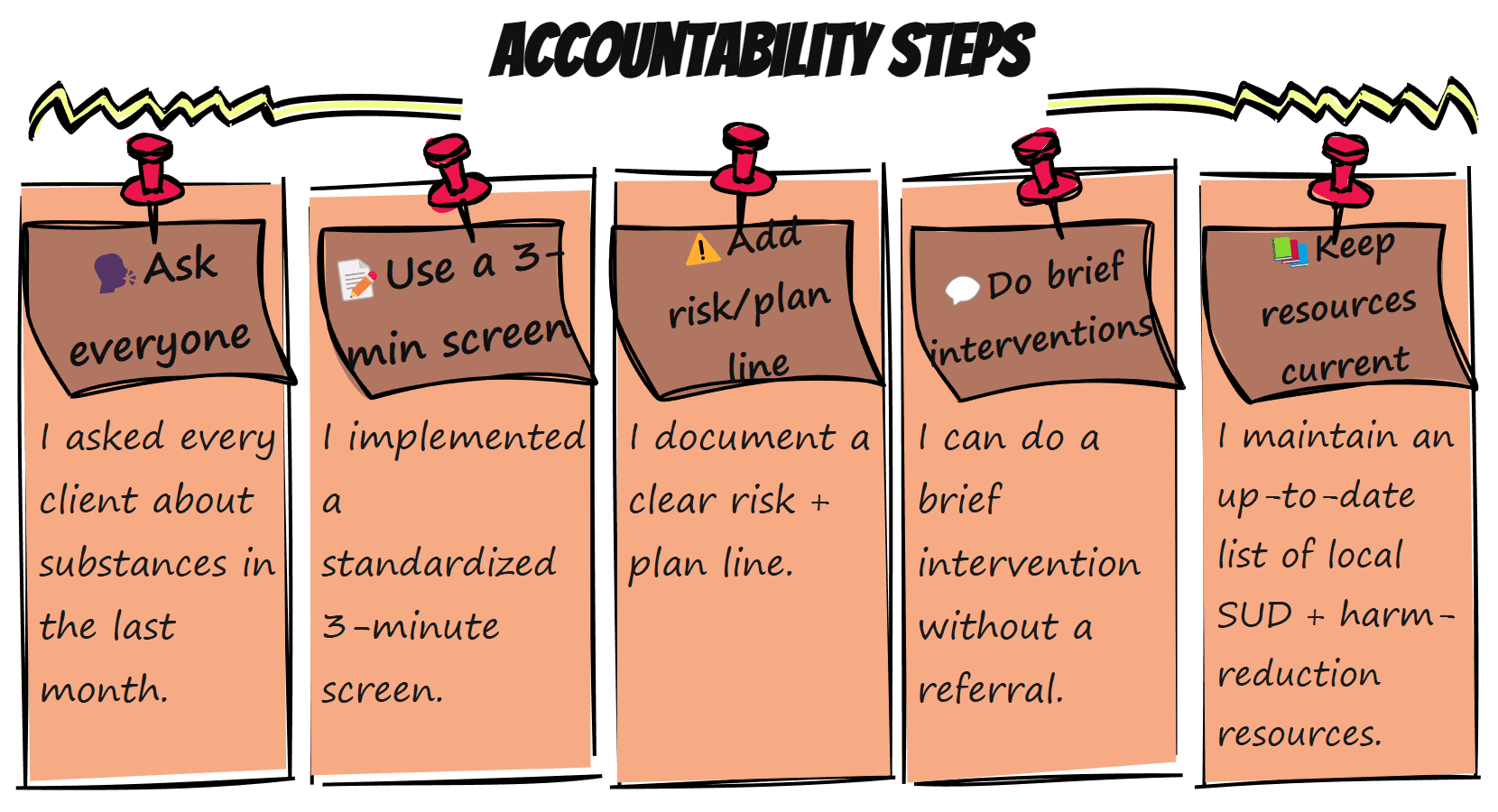
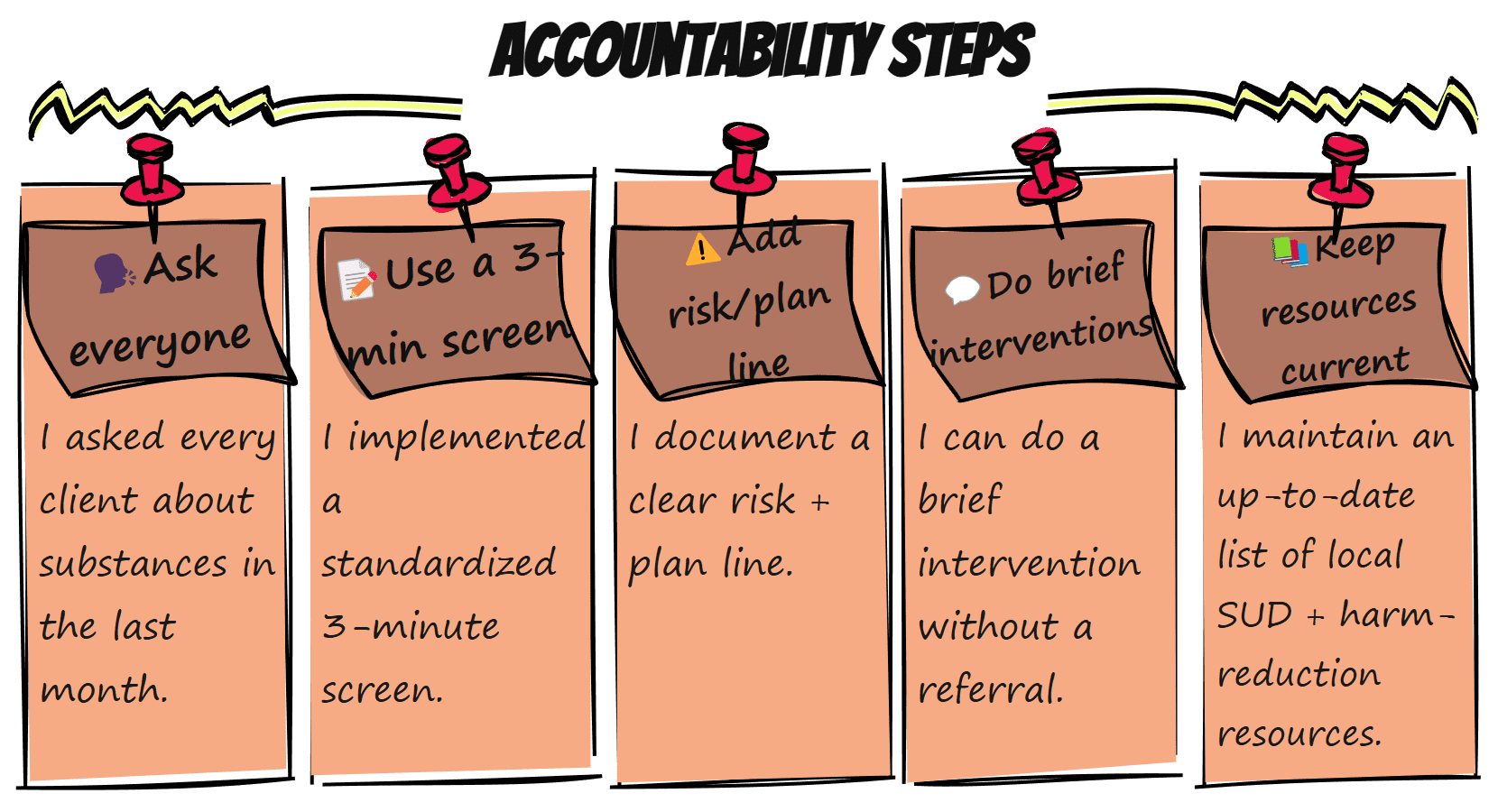
Accountability Check: Are You Caught in an Intake Illusion?
Before we move on, let’s turn the lens on our own process.
- I asked every client about substances in the last month.
- My template includes a 3-minute screen and a risk/plan line.
- I can do a brief intervention without a referral (SBIRT refresher).
- I have a current list of local SUD and harm-reduction resources (plus FindTreatment.gov and 988 Lifeline).
If you can’t tick these yet, that’s your next clinical growth edge—not a failure. Bookmark this post and pick one micro-change for your next three intakes.
Prefer a one-page reminder? Download/print the “Accountability Steps” mini-poster below and pin it near your intake notes. It’s sized for 8.5×11 and works as a quick self-audit before every intake.
When a screen is positive—or even uncertain—having client-ready handouts within reach keeps momentum going.
Resources You Can Share with Clients During a SUD Screening
- “Safer Use” one-pager (alcohol + cannabis basics)
- Cravings plan (3 things to do, 3 people to text, 3 places to go)
- Medication safety (no mixing with benzos/opioids; lockbox for stimulants/opioids)
(Clinician references: NIAAA, NIDA, CDC Naloxone, FDA safety communications.)
Join the Conversation: Have you caught yourself in one of these illusions? What helped you start asking every time? Share a quick story below or in our peer group—your small change may become someone else’s big shift.
💛 Keep showing up,
Stephanie | The Underrated Superhero
Prefer a one-page reminder? Print the “Accountability Steps” mini-poster below and pin it near your intake notes (8.5×11).