Quick take: Silence isn’t absence—it’s data. During intake, pauses, topic pivots, or “not really” answers often mark risk and uncertainty, not “no use.” A short, normalized screen + a couple of bridges can protect rapport and surface what matters. (That’s the SBIRT spirit: SUD Screen → brief intervention → referral as needed.
Missed Blog #2? Read The Intake Illusion: SUD Screening at Intake
Why silence shows up in SUD Screening
Most of the time, silence clusters around fear—fear of losing their job, their kids, their insurance. Sometimes it’s shame (“good clients don’t use substances”). Other times clients genuinely don’t know if you’re asking for therapy reasons, medical reasons, or whether this information could end up somewhere they don’t want it. And sometimes a client’s nervous system is so activated that they can barely string sentences together, let alone talk about something this loaded.
Bottom line: silence is a signal to swap formats (self-administered or checklist), not a reason to skip the screen. Validated micro-screens make this quick: NIAAA SASQ for alcohol; NIDA Quick Screen → TAPS for multi-substance; CRAFFT 2.1 for adolescents; WHO ASSIST if you need more structure.
The “quiet” you’ll actually see
You’ll notice the long pause when you mention alcohol, or how they suddenly want to talk about their work schedule instead. “Not really” becomes their favorite phrase—but they can’t give you examples of what “not really” looks like. Sometimes they’ll ask if they can just fill out a form instead of talking about it.
A silence-aware 3-minute SUD Screen (SBIRT-friendly)
0:00–0:10 — Set the frame
“I ask everyone a few quick questions about alcohol, cannabis, and medications so I can match care. Okay to do that now?”
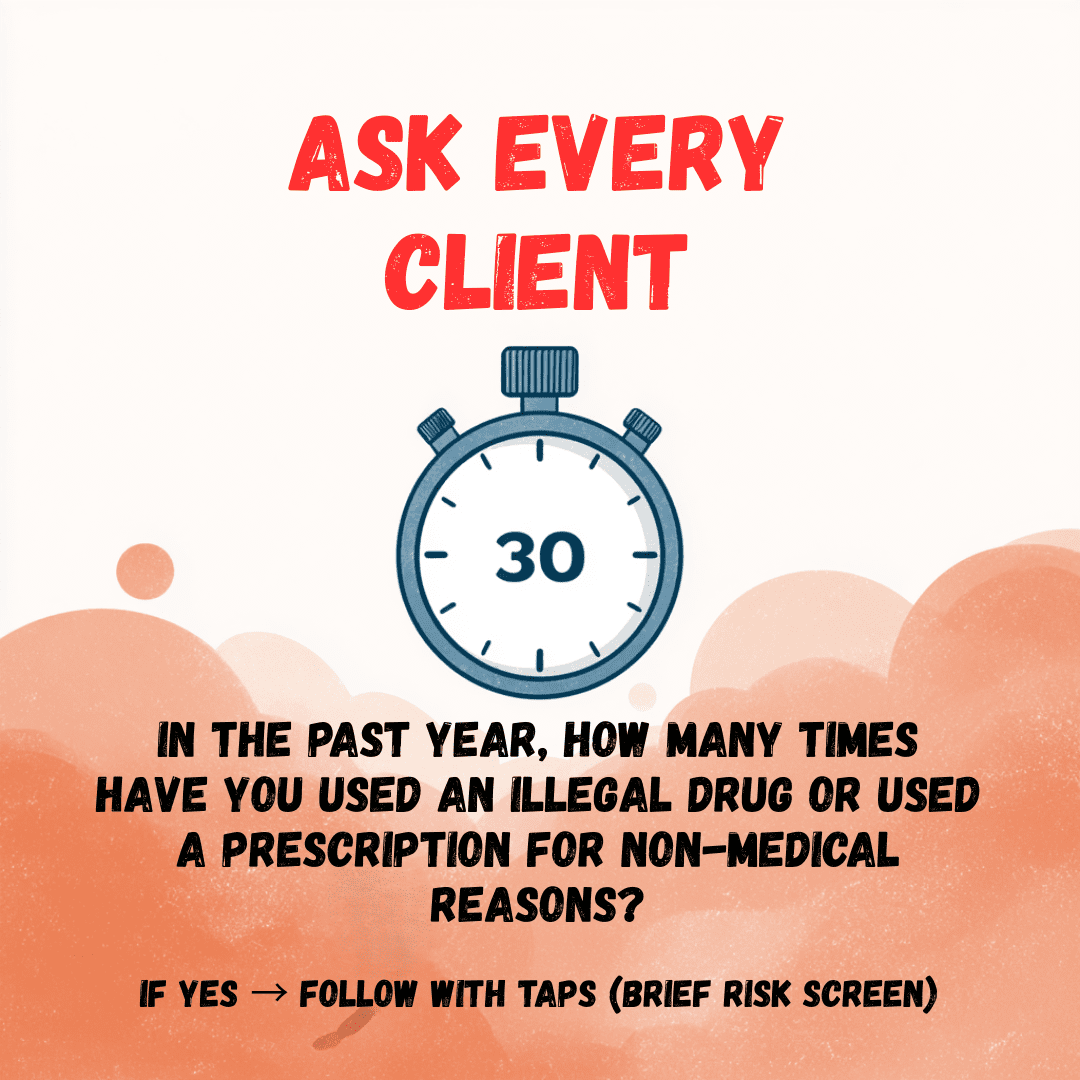
0:10–1:00 — Prescreen & single items
- Alcohol: “How many times in the past year did you have 4+ (women) / 5+ (men) drinks in a day?” (≥1 = follow-up). (NIAAA SASQ.) Then, expand if needed.
- If alcohol negative or uncertain: use the NIDA Quick Screen (past-year frequency across alcohol/tobacco/prescription misuse/other drugs). When any use is acknowledged, next run TAPS for brief risk stratification.
The client may go quiet (at any point), if they do, offer a bridge:
- “It’s okay if that’s hard to answer out loud. Want to do a quick checklist and hand it back?”
- “Some people prefer yes/no; others write it. What’s easier?”
- “A lot of people report occasional heavy drinking or mixing meds by accident—what fits even a little?”
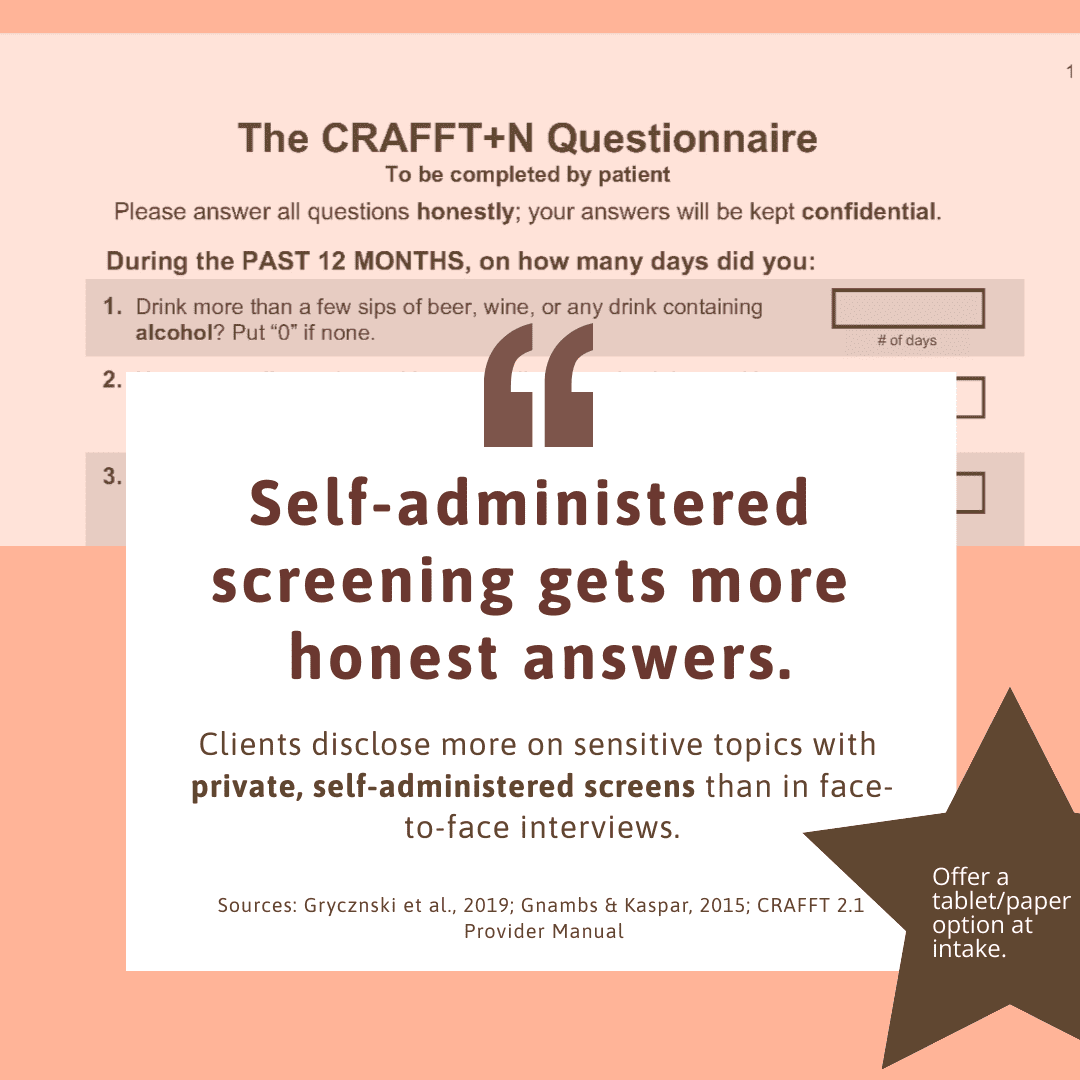
Clients disclose more with private, self-admin screens than face-to-face interviews.
Sources: Gryczynski et al., 2019; Gnambs & Kaspar, 2015; CRAFFT 2.1 Provider Manual.
1:00–2:15 — Clarify & function (only if positive/uncertain)
“What does a typical week look like? Any mixing with meds or days it’s more than intended? What do you hope it helps with?”
2:15–3:00 — Safety & next step
Menu it: safer-use tweak, cravings plan, brief counseling, or warm referral. (This is the “BI” part of SBIRT.)
Adolescents? Use CRAFFT 2.1 (self-administered works well for silence).
Adults & alcohol? Routine screening + brief counseling is recommended by USPSTF (keep it simple with SASQ or AUDIT-C).
Run the 2-minute Brief Substance Use Checklist
For clinicians. Client self- or clinician-administered.
–Chart-ready note line included
–Per-item guidance as you go
–Final summary + downloadable PDF (de-identified)
SBIRT-aligned triage: mild · moderate · considerable concern
[Start online] [Print version]
Educational tool; not medical advice.
Access note: Interactive tools (e.g., the Brief Substance Use Checklist) require at least free account to ensure you can save, print, and re-download client-ready summaries.
Prefer offline? Use the printable checklist (PDF) instead.
Four micro-scripts for common silence moments during SUD SCreening
1) The long pause
“Take your time. Many people use more than they plan. What’s been true for you recently?”
2) The topic pivot
“We’ll get to scheduling, yes. One quick box first—any days of 4/5+ drinks, cannabis use, or extra meds lately?”
3) ‘Not really’
“When you say ‘not really,’ what does that look like in a week—one day, two, none?”
4) ‘I’d rather not answer’
“Totally okay. Choose: we can mark ‘prefer not to say’ and circle back, or you can tick a private checklist.”
Red flags where silence matters even more
In particular, take a closer look when you notice:
- Sedative or stimulant prescriptions with vague “falls” or “can’t sleep.”
- Repeated Monday no-shows, injuries without details, or night sweats “from anxiety.”
- Respiratory issues with heavy vape/smoke exposure “not discussed.”
Silence + any of these = complete a validated screen and offer a micro-intervention. (USPSTF endorses adult alcohol screening; for broader substances, Quick Screen → TAPS is fast.)
First-session micro-interventions (≤5 minutes)
Meanwhile, you can still support change in under five minutes:
- Reflect + scale: “On 0–10, how important is it to keep use from getting in the way of your goals?”
- Link to what matters: “You named sleep/parenting/work—how does use help…and complicate it?”
- Pick one next step: safer-use tweak (no mixing with benzos/opioids; hydration; ride plan), cravings plan (3/3/3), or a warm referral.
- If indicated: consider ASSIST for more structure or plan a focused follow-up.
Charting line you can paste for SUD Screening
“Brief SUD screen completed (SASQ / Quick Screen→TAPS as indicated). Client preferred [verbal/self-admin]. Reviewed frequency/amount/route, risks (e.g., mixing with meds, driving). Brief counseling provided; plan = [safer-use step / cravings plan / referral]. Follow-up scheduled.”
(CODING NOTE: SBIRT has defined service codes; check your setting’s rules.)
Common pitfalls in SUD Screening → tiny fixes
Pitfall: Treating silence like “no.”
Fix: Offer an alternate format, then return later.
Pitfall: Deferring to “someone else covers it.”
Fix: Division of labor ≠ duplication—brief screens are collaborative across disciplines. (That’s SBIRT.
Resources you can hand to clients (pairs with silence moments) after SUD Screening
- Conversation Starter Guide (neutral openers + micro-scripts)
- Safer Use one-pager (alcohol & cannabis basics)
- Cravings Plan (3/3/3)
- Medication Safety (boxed-warning highlights; lockbox guidance)
Grab them free: create a free account for instant links + flipbook.
Accountability check
Before you close, make sure your intake consistently covers the basics:
- Include SASQ (adults) and CRAFFT (youth) in your intake template.
- Offer a self-admin fallback when clients go quiet.
- Document a brief plan—even when disclosure is partial.
- End with one micro-step the client will try this week..
💬 Join the conversation: What “silence moment” shows up most in your intakes—and which bridge line are you committing to this week? Drop it below or share in the peer group.
📥 Free tools: Conversation Starter Guide • Safer Use • Cravings Plan (3/3/3) • Medication Safety
Create your free account for instant links + flipbook.
💛 Keep showing up,
Stephanie | The Underrated Superhero