High Caseload Management for Clinicians
The number was 32.
Thirty-two progress notes I needed to write. I remember staring at that number and feeling like a freight train just hit me. I’d been handling everything so well—sessions running smoothly, clients engaged, groups productive. But the notes. No matter how efficient I got, notes still took time. And when you’re carrying 80+ clients, the math eventually catches up with you.
If you’ve ever looked at your to-do list, your caseload, your schedule—and felt your chest tighten because there’s no possible way to get it all done—this post is for you.
📚 This is Blog #13 in the New Clinician Survival Kit Series (Click to explore the series)
Weekly honest support for the struggles every clinician faces: “I hate group therapy.” “I can’t do this.” “My client hates me.” “I’m making it worse.” “I can’t say no.” “They’re going to report me.” “I’m too tired to care.” “What do I even say?” “I don’t know enough.” “They keep relapsing.” “Am I documenting wrong?” “My supervisor doesn’t get it.” “I can’t handle this caseload.”
These aren’t signs you’re failing. They’re signs you’re human.
The Math That Doesn’t Add Up
Let me tell you what 80+ clients actually looked like.
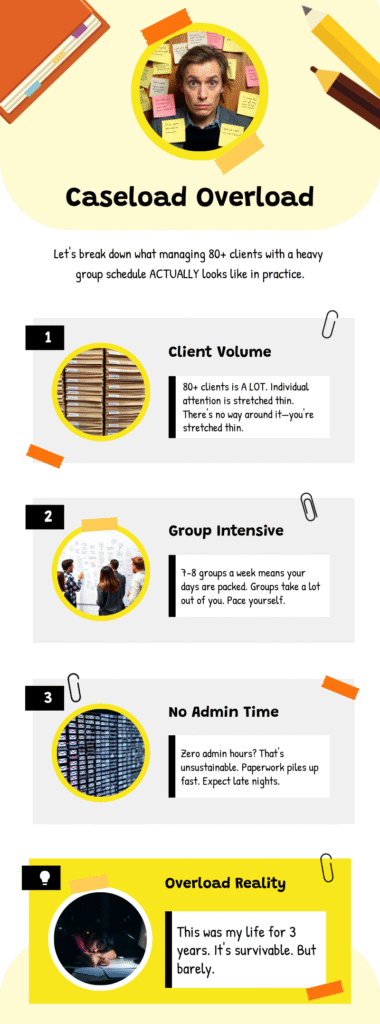
I was running 7-8 groups every week. That was the only way I could see that many people—there’s no universe where I could manage 80 individual sessions. So I designed my schedule around groups: 2-3 groups a day, four days a week. Then I’d fill in with a mix of virtual and in-person individuals around them.
Here’s what nobody tells you about high caseloads: the sessions aren’t the hard part. I loved my groups. I was good at them. The clients showed up because I had solid relationships with them.
The hard part is everything after the session ends.
I never scheduled time for admin work. I’d do documentation during no-shows, in the cracks between sessions, or—more often than I want to admit—cutting into my own time. My own sleep. My own sanity.
For three years, I worked two jobs. Eighty hours a week. And the cycle looked like this: work until I couldn’t anymore, burst into tears, cry to my husband, go to sleep, wake up, do it again.
“Just Slow Down”
Here’s the thing I need to admit: my supervisors were actually pretty good about this. When I told them I was overwhelmed, they acknowledged it. They were empathetic. They told me to slow down.
The problem was me.
I couldn’t say no to new referrals. Every time someone needed services, I’d take them on. Part of it was genuine care—these were real people who needed help. Part of it was some mix of ego and work ethic that made me believe I could handle anything if I just worked harder, got more efficient, built better systems.
So if you’re reading this and blaming your agency or your supervisor for your caseload—maybe that’s true. But ask yourself: are you part of the problem too? Are you the one who can’t turn down referrals? The one who keeps saying yes when you should say no?
I was. And owning that was the first step toward doing something about it.
High Caseload Management for Clinicians: What Actually Kept Me Afloat
I’m not going to pretend I had some magical solution that made 80 clients feel like 20. It was hard. It was exhausting. But I did have systems that kept me from completely drowning. Well—mostly kept me from drowning.

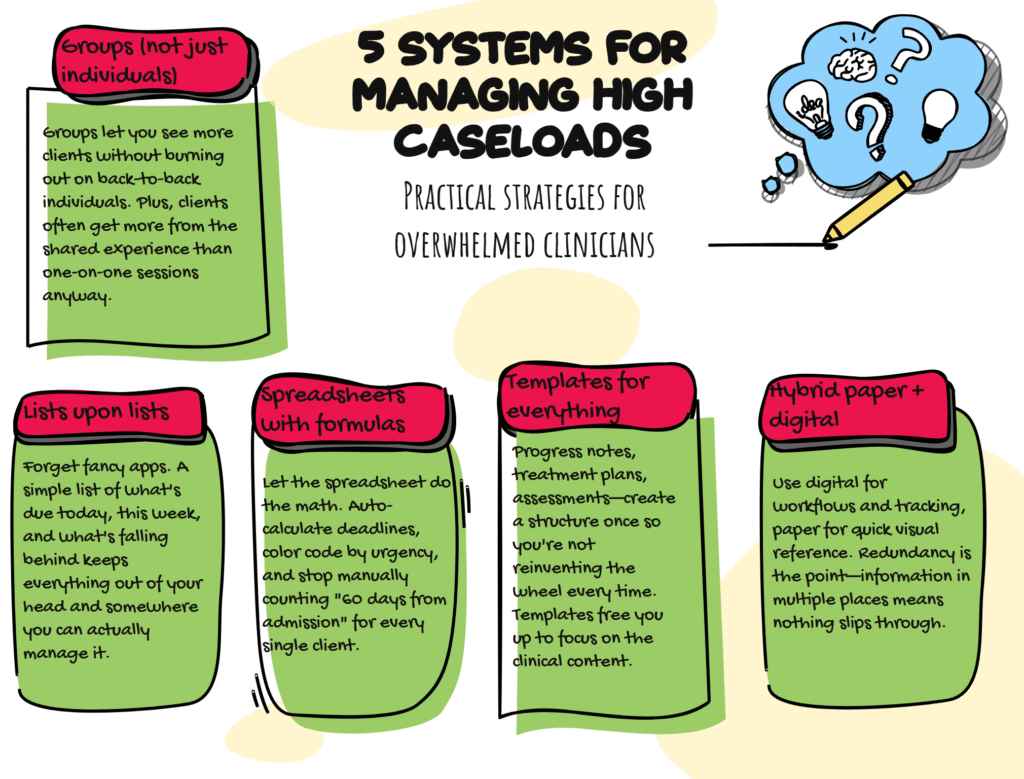
Groups Were the Answer
I designed my practice around them intentionally because that was the only way to maximize the number of clients I could actually see. Every time my individual caseload started creeping too high, I’d consider starting another group. This wasn’t just survival math—I genuinely loved groups, and clients often got more out of them than individual sessions anyway.
Groups weren’t plan B. They were the only math that worked.
Systems That Kept Me Afloat
Lists upon lists upon lists. I lived by my lists. Not fancy apps or complicated project management systems—just lists. What needed to happen today. What was due this week. What was falling behind. The act of writing it down got it out of my head and onto paper where I could actually deal with it.
Spreadsheets that did the math for me. I had tracking systems with formulas that automatically calculated when treatment plans were due, when reviews were coming up, when clients were approaching compliance deadlines. Color coding was everything—red for urgent, yellow for coming soon, green for done. Instead of manually calculating “60 days from admission date” for every single client, the spreadsheet did it. I just had to look at what was red.
The Backup Plan
Templates that saved my sanity. I created templates for everything—progress notes, treatment plans, assessments. Not to phone it in, but because recreating the wheel for every single document when you have 80 clients will break you. Templates gave me structure so I could focus on the actual clinical stuff instead of formatting.
A hybrid system. I used my iPad for client interactions and digital workflows, but I also kept paper tracking sheets with color coding for quick visual reference. The redundancy was on purpose—information in multiple places meant nothing fell through the cracks.
📊 The High-Caseload Success Guide: Documentation Systems for Overworked Clinicians (Click to preview)
How I Managed 80+ Clients with Top Retention Rates
This comprehensive guide includes the exact systems I used to stay organized while managing a high caseload without burning out:
- Digital Mastery — iPad workflows and EHR optimization
- Strategic Information Management — tracking systems with color-coding
- Efficiency Through Templates — reduce documentation time without sacrificing quality
- Bulletproof Workflows — checklists that prevent compliance gaps
- Consistent Metrics Tracking — quarterly benchmarks for sustainable productivity
- Client Engagement Techniques — retention strategies that actually work
✓ Included with your free membership — No additional signup required
The One Thing I Wouldn’t Do Again
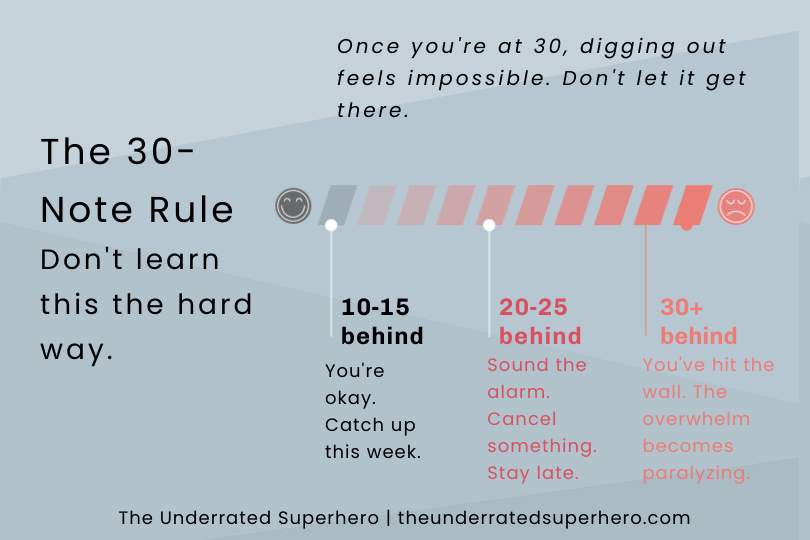
Don’t let your notes pile up past 30.
I mean it. When I hit 30+ notes behind, it was like hitting a wall. The overwhelm became paralyzing. It stopped being “I’m a little behind” and turned into “I don’t even know where to start.” And that kind of backlog isn’t good for audits, for compliance, for your anxiety, or for the quality of your documentation.
Somewhere around 20-25 notes behind, sound the alarm. Cancel something. Stay late. Come in early. Do whatever you have to do to not let it hit 30. Because once you’re there, digging out feels impossible.
📝 The Tool That Keeps Notes From Piling Up
The Quick Capture Cards give you a 60-second system for capturing what happened immediately after each session. Circle keywords, jot key phrases—then write the full note later without losing critical details. It’s the difference between “I vaguely remember this session” and “I have everything I need right here.”
What I’d Tell You Right Now

If you just got assigned your 40th client and you’re panicking, here’s what I want you to do:
Take five minutes. Just five. Breathe.
Then muster up your must-haves. For me, it was putting on my favorite show in the background, grabbing my favorite drink, and getting as comfortable as possible at my desk (or at home if I was working late). Set yourself up so the hard work sucks a little less.
Then start with one thing. Not the whole list. One note. One phone call. One treatment plan. Just one.
That’s it. That’s the whole strategy when you’re drowning: get comfortable, get started, do one thing. Then do the next thing. Lists will save your life because they let you stop thinking about everything and just focus on what’s next.
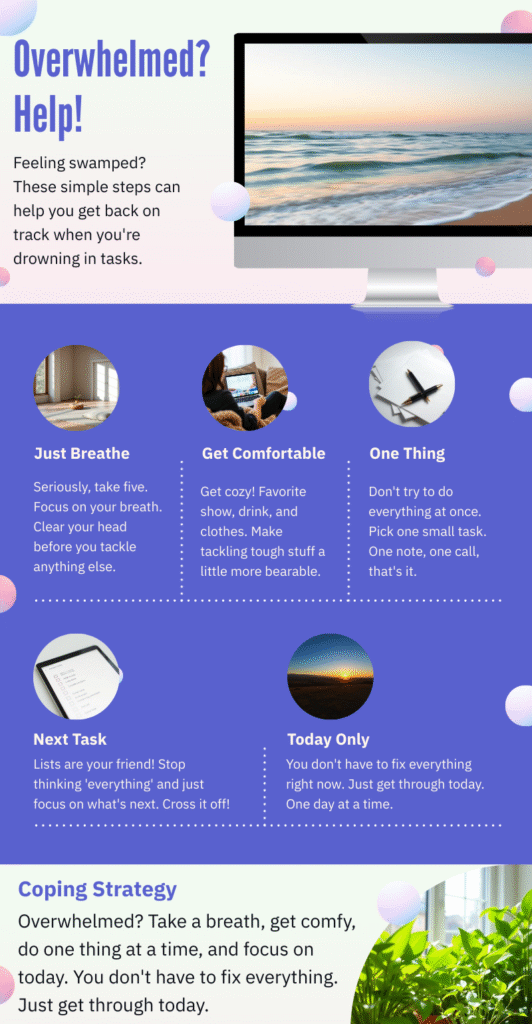
You don’t have to solve the systemic problem of your caseload right now. You just have to get through today.
The Harder Conversation
I managed 80+ clients with top retention rates for years. I had the highest productivity numbers. Hit every metric. By most measures, I was thriving.
I was also crying to my husband regularly and waking up exhausted to do it all again.
Both things were true.
📊 The Numbers Behind the Overwhelm
- 93% of behavioral health workers report experiencing burnout
- 48% are considering leaving the field due to workforce shortages
- 33% annual turnover rate for substance abuse counselors
- 43 of 44 states reported behavioral health workforce shortages in 2024
Sources: National Council for Mental Wellbeing, PMC Research, NRI State Reports

High caseloads in addiction treatment aren’t a badge of honor. They’re usually a symptom of underfunded systems, high turnover, and agencies that would rather burn through clinicians than hire enough staff. You can be excellent at your job AND be in an unsustainable situation. Those aren’t contradictions.
If you’re managing an impossible caseload right now, I want you to know you’re not bad at your job. You’re probably under-resourced and over-assigned. The systems I shared can help you survive it. But surviving isn’t the same as thriving.
At some point, you might need to have the harder conversation—with your supervisor, with yourself—about what’s actually sustainable. Not today, maybe. Today you just need to get through your to-do list.
But eventually.
You’re Not Alone in This
Every clinician I know has felt crushed by their caseload at some point. The panic when you look at your schedule. Guilt when stuff slips. That exhaustion that just… doesn’t go away.
These aren’t signs you’re failing. They’re signs the system is asking too much. And while we can’t fix the system overnight, we can share what works, build better tools, and remind each other we’re not alone.
What’s your caseload reality right now? What’s helping you stay afloat? Drop a comment—I’d genuinely love to know.
Next Week: We’re tackling another brutal truth that keeps clinicians up at night. See you then!
Until Next Week | The Underrated Superhero
© 2025 The Underrated Superhero LLC. All Rights Reserved.
📖 External Resources & Research
- 🔗 National Council: Behavioral Health Workforce Study — 93% of behavioral health workers report experiencing burnout; 48% considering leaving due to workforce shortages
- 🔗 PMC Research: Staff Turnover in Substance Abuse Treatment — Annual turnover rates of 19-50% among addiction counselors; turnover increases caseloads for remaining staff
- 🔗 PMC Research: Burnout Among Substance Abuse Counselors — Rural vs. urban comparison of causes, consequences, and prevention strategies
- 🔗 SAMHSA: Behavioral Health Workforce — Federal resources for workforce development and burnout prevention
- 🔗 SAMHSA: Addressing Burnout Through Organizational Strategies — Evidence-based organizational approaches to reduce clinician burnout
🛠️ Resources from The Underrated Superhero
- 📊 High-Caseload Success Guide — The complete 6-system framework I used to manage 80+ clients with top retention rates. Includes Digital Mastery, Strategic Information Management, Templates, Workflows, Metrics Tracking, and Client Engagement systems. Free with membership.
- 📝 Quick Capture Session Cards (PDF) — The 60-second documentation system that keeps notes from piling up. Circle keywords, jot key phrases, write the full note later. Free PDF download. | Shop pre-printed cardstock →
- 🛠️ The Sidekick: Documentation Mastery Kit — Quarterly tools for building sustainable documentation systems, including the 12-month Documentation Mastery Planner
- 📧 Subscribe to the New Clinician Survival Kit Series — Weekly honest support for the struggles every clinician faces—no fluff, no toxic positivity
Previous Posts in the New Clinician Survival Kit Series
- 📖 Am I Documenting Wrong? When Compliance Anxiety Takes Over
- 📖 They Keep Relapsing: When Recovery Doesn’t Look Like You Expected
- 📖 I Don’t Know Enough: When School Didn’t Prepare You for This
See all posts in the New Clinician Survival Kit Series