Documentation for Therapists
You submit the note. Then you reopen it. Read it again. Check for blanks. Check for errors. Close it. Open it one more time just to be sure.
I used to do this with everything. Double and triple check every document, even toward the end of my career. My professor drilled it into us early—improper documentation, blanks left unfilled, bias in your writing—these things have consequences. Audits. Legal proceedings. Client care. So, I learned to be obsessive about it.
I wrote about a related fear in “They’re Going to Report Me”. But documentation anxiety is its own beast. You’re not just worried about getting in trouble—you genuinely don’t know what “good enough” looks like. Because nobody taught you.
📚 This is Blog #11 in the New Clinician Survival Kit Series (Click to explore the series)
Weekly honest support for the struggles every clinician faces: “I hate group therapy.” “I can’t do this.” “My client hates me.” “I’m making it worse.” “I can’t say no.” “They’re going to report me.” “I’m too tired to care.” “What do I even say?” “I don’t know enough.” “They keep relapsing.” “Am I documenting wrong?”
These aren’t signs you’re failing. They’re signs you’re human.
What School Didn’t Cover
My program briefly touched on intakes and treatment plans. That was about it.
Nobody taught me how to write court-ordered evaluations. Nobody explained what to include (or leave out) when a probation officer requests information. Progress notes? I had to figure out what actually needed to be in there through trial and error.
Collateral communication with schools, social workers, attorneys—I learned that on the job, made mistakes, and eventually built my own systems so I’d stop messing it up. helping anyone? I asked myself that more times than I’d like to admit.
The Mistakes I Keep Seeing
After years of supervising and reviewing other clinicians’ documentation, the same stuff comes up constantly:
Blanks. Every field needs something. Even “N/A” is better than empty. A blank looks incomplete at best, negligent at worst.
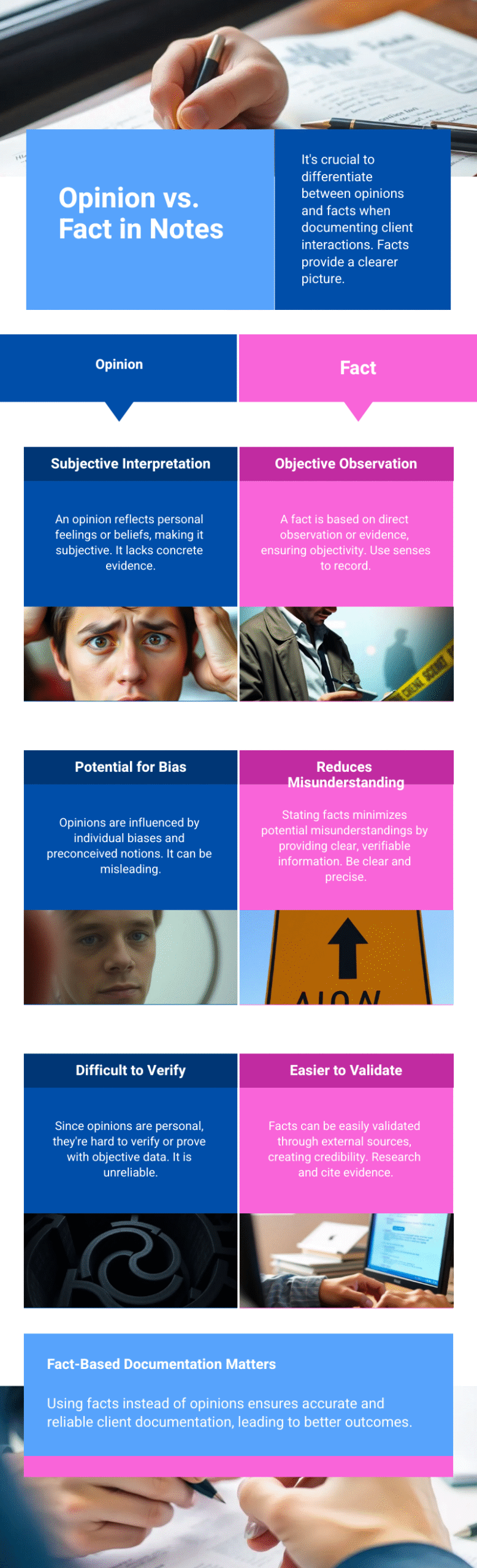
Opinion disguised as fact. “Client seemed unmotivated” is your interpretation. “Client stated he doesn’t see the point of treatment” is what happened. Write what you observed and what they said. Not what you assumed.
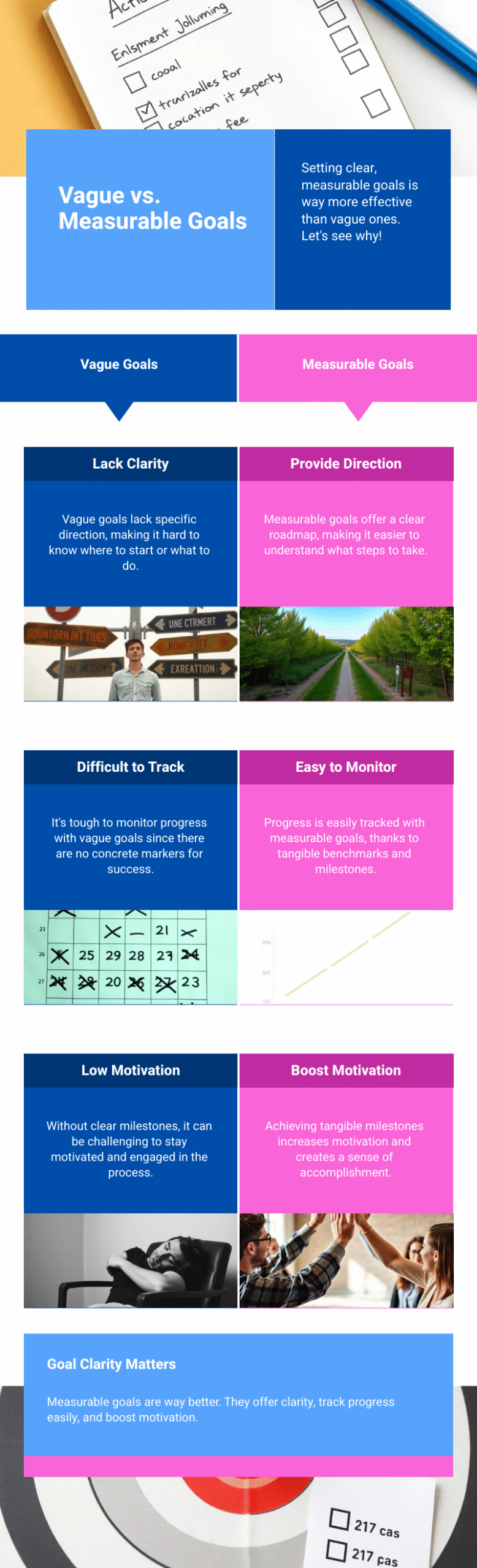
Vague treatment goals. “Client will work on relapse prevention” tells me nothing. “Client will create and revise a written relapse prevention plan identifying three high-risk situations and coping strategies” gives me something I can actually measure.
Missing justification. Why is this person in treatment? What’s the medical necessity? If it’s not documented, it didn’t happen. You can’t bill for it. Check your state’s documentation standards—in Illinois, that’s IAODAPCA. Other states have their own credentialing bodies and audit guidelines.
Missing what actually happened in session. Your note should reflect what occurred. Not what you planned. Not what you hope to cover next time. What you actually did.
Skipping stage of change. This gets missed constantly, and it matters for treatment planning.
Collateral Communication: Stop Oversharing

When probation officers, courts, or social workers request information, new clinicians tend to send way too much.
You don’t need to attach your intake. You don’t need to forward your full assessment. You don’t need a three-page letter explaining everything.
What they usually need:
- Is the client attending?
- Are they engaging?
- Are they testing negative (or denying use)?
- Are they making progress?
That’s it. Keep it minimal. Protect your client while satisfying the request.
I’ve seen letters from other clinicians that go on forever. I don’t know why. More is not better here. I created a Probation Communication Forms System specifically because I got tired of watching people overcomplicate this.
AI and Documentation: Read Before You Submit
A lot of clinicians use AI for progress notes now. Fine. I’ve done it too.
But here’s the problem: you prompt it to write a note about “individual session on relapse prevention” and it generates content about coping skills, triggers, and interventions you never actually covered. If you don’t read carefully, you’re billing for services you didn’t provide.
That’s not just a compliance issue. It’s an ethics issue. The NAADAC Code of Ethics is clear on accurate documentation.
When I used AI for notes, I had to give a lot of detail before generating anything—and I still reviewed every note before submitting. Sometimes it needed significant revision. AI can help, but it’s not a replacement for actually knowing what happened in the session.
How I Stopped the Anxiety Spiral
I got tired of triple-checking everything. So I built systems that did the checking for me.
Templates with required fields already built in. Checklists for different document types. To-do lists that tracked what still needed signatures or reviews.
It sounds like overkill, but it actually made things easier. Instead of running through everything mentally—did I include stage of change? did I justify medical necessity? are there blanks?—I had a structure that caught it.
That’s eventually why I started creating documentation templates for other clinicians. I figured this stuff out the hard way. No reason you should have to.
If you want a complete system—templates, checklists, workflows—I put it all together in the Documentation Mastery Sidekick Kit, Fall 2025 Version.
Quick Self-Audit Before You Submit
📋 Documentation Self-Audit Checklist Run through this before you submit anything. (Click to expand)
Run through this:
- No blanks (or N/A where something isn’t applicable)
- Fact-based language, not interpretation
- Measurable goals
- Medical necessity justified
- Stage of change documented
- What happened in session is clear
- Collateral communication is minimal
- If AI-generated, reviewed for accuracy
The Anxiety Doesn’t Fully Go Away
I’m not going to tell you that once you have a system, you’ll never worry again. That’s not true.
But the anxiety drops. You stop reopening notes four times. You stop spiraling before audits. You know what’s in there because your process catches the gaps.
It’s not about being perfect. It’s about having a structure that makes “good enough” actually feel good enough.

Next Week: We’re tackling another brutal truth that keeps clinicians up at night. See you then!
Until Next Week | The Underrated Superhero
© 2025 The Underrated Superhero LLC. All Rights Reserved.
Resources Referenced in This Post
- IAODAPCA (Illinois Alcohol and Other Drug Abuse Professional Certifying Association) – State credentialing body with documentation standards and audit guidelines. Counselors in other states should check their own state credentialing boards for specific requirements.
https://www.iaodapca.org/ - NAADAC Code of Ethics – Professional standards for addiction counselors including documentation accuracy, billing practices, and ethical responsibilities
https://www.naadac.org/code-of-ethics
Additional Support from The Underrated Superhero
- 📝 Probation Communication Forms System – Free templates for collateral communication that give POs what they need without oversharing
- 📋 Documentation Templates Library – Intake, treatment plan, and progress note templates with required fields built in
- 🎯 Documentation Mastery Sidekick Kit – Complete system with templates, checklists, and workflows to eliminate the triple-checking spiral
- 🛠️ Free Clinical Tools – Downloadable resources to support your clinical work. Requires free account.
Previous Posts in the New Clinician Survival Kit Series
- 📖 They’re Going to Report Me: Professional Fear and Compliance Anxiety
- 📖 I’m Making It Worse: Fear of Harming Clients
- 📖 I Can’t Do This: When Imposter Syndrome for Therapists Hits Hardest
See all posts in the New Clinician Survival Kit Series