Clinical Supervision for New Counselors
In grad school they talk about supervision like it’s going to be this transformative experience. A wise, experienced clinician guiding you through your hardest cases. You leave every session feeling supported and better equipped.
Then you get your first supervisor.
And it’s… not that.
You’re not imagining it. Research shows that 93% of supervisees report currently receiving inadequate supervision, and 35.3% report receiving supervision that is actually harmful Sage Journals (Ellis et al., 2014). That’s not a small number of people having a bad day. That’s a systemic problem.
📚 This is Blog #12 in the New Clinician Survival Kit Series (Click to explore the series)
Weekly honest support for the struggles every clinician faces: “I hate group therapy.” “I can’t do this.” “My client hates me.” “I’m making it worse.” “I can’t say no.” “They’re going to report me.” “I’m too tired to care.” “What do I even say?” “I don’t know enough.” “They keep relapsing.” “Am I documenting wrong?” “My supervisor doesn’t get it.”
These aren’t signs you’re failing. They’re signs you’re human.
My First Experience with Clinical Supervision for New Counselors
My first clinical supervisor blurred boundaries constantly. One minute we were acting like friends—or even mother and daughter—and the next she was disciplining me, questioning why I was talking to certain staff, asking why I was applying for other jobs.
Confusing. Unprofessional. I never knew which version of her I was getting.
She also had a master’s degree but struggled with writing and was completely lost when it came to technology. I know that sounds petty. But it affected how I saw her competence. And once I started questioning that, I couldn’t fully respect her anymore—or hear what she was trying to teach me.
Here’s the part I don’t love admitting she did try. She had strengths I didn’t bother to see because I was so focused on what she couldn’t do. I checked out. Wrote her off.
Looking back, I probably could’ve gotten more out of it than I did. I’m not saying she was great. But I didn’t exactly show up ready to learn either.
The Next One Was Different—Still Not Right Though
When I moved to the adolescent substance abuse section of the health department, I got a new supervisor. She wasn’t passionate about addiction work. Wasn’t experienced in it either. But weirdly, I felt more supported.
I knew I could go to her in a crisis. I didn’t feel so alone.
It wasn’t the clinical mentorship I wanted. But it was stable. And honestly? Sometimes that matters more than expertise.
The Real Problem with Clinical Supervision for New Counselors

Here’s what followed me through basically every job I had: I never got supervision from someone who really knew addiction.
Most of my supervisors were mental health clinicians who’d moved into leadership. And that’s just how it goes at a lot of agencies—if you want to advance, you move away from SUD treatment. So, the people supervising addiction counselors are often people who haven’t done the work. Or haven’t done it in years.
This isn’t just my experience. A NAADAC survey found that a significant percentage of substance abuse counselors receive no clinical supervision at all NCBI—and among those who do, many report inconsistent experiences.
Which meant I was figuring out addiction-specific stuff mostly on my own. Treatment planning for someone in active use. Navigating MAT when your agency has strong opinions about it. What to do when a client relapses for the fifth time and you’re not sure anymore if you’re helping.
Nobody in supervision was walking me through any of that.
The research backs this up: when mental health counselors have limited and/or inadequate training in substance use disorders, effective clinical supervision may advance their professional development PubMed Central—but that assumes the supervisor actually knows SUD work. When they don’t, you’re on your own.
What Actually Helped When Clinical Supervision for New Counselors Failed
My colleague.
We consulted on everything. Clients, cases, ethical gray areas, “what would you do if” scenarios. We debriefed hard sessions. We vented. We figured it out together.
That peer relationship taught me more than any formal supervision I received.
My colleague taught me more than any formal supervision I received. Peer support isn’t plan B. Sometimes it’s the whole plan.


What I’d Tell a New Clinician Dealing with This
Two things.
First—try to look past your criticisms.
I’m not saying ignore red flags. If your supervisor is crossing boundaries, bringing their own mess into your sessions, or making things worse instead of better—that’s real. That’s bad supervision and you’re not imagining it.
But if it’s more like… they’re just not what you hoped for? They don’t know addiction? They’re fine but not helpful?
Try to find what they can offer. I wrote off my first supervisor too fast. Focused on what she couldn’t do and missed whatever she could. I do regret that.
Second—go find what you need somewhere else.
Don’t wait around hoping your supervisor suddenly becomes the mentor you wanted. Build your own support:
- A colleague you trust (this saved me)
- Peer consultation, even informal
- Networking with other addiction counselors who actually get it
- Online communities and resources
- Trainings that go deeper than your agency provides
If you want structure for those supervision conversations you are having, the Supervision Prep Notepad in the Fall 2025 Survival Kit can help you organize your thoughts before you walk in—so you get something useful out of even imperfect supervision.
You’re allowed to supplement. You’re allowed to get your needs met even if supervision isn’t meeting them.
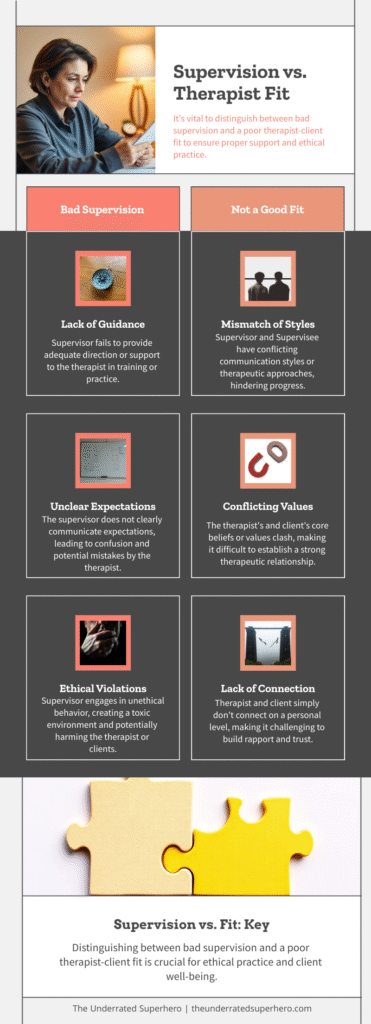
Bad Supervision vs. Just Not a Good Fit
These aren’t the same thing.
Bad supervision:
- Boundary problems
- They’re bringing their own stuff into your sessions
- Drama, chaos, unprofessionalism
- You feel worse after supervision than before
- You’re worried about their ethics, not just their style
Not a good fit:
- Hard to pinpoint what’s wrong exactly
- They’re competent, just not in what you need
- You’re not clicking even though they’re trying
- You’re not growing but you’re also not being harmed
Both are frustrating. But one might need escalating or documenting or getting out. The other just means you need to build support elsewhere while taking what you can from what’s there.
Research on effective supervision shows that most aspects of effective clinical supervision are related to SUD counselor job performance PubMed Central—which means when supervision works, it really works. When it doesn’t, you feel it in your clinical work too.
🔍 Signs Your Supervision Isn’t Working (Click to take the self-check)
Check any that apply to your current supervision experience:
If you checked 3 or more: It might be time to supplement your supervision with other support. That’s not failure—that’s resourcefulness.
When Clinical Supervision for New Counselors Isn’t Working

New clinicians need more support than most agencies are set up to give. The people supervising addiction work often haven’t done addiction work in a long time—if ever. That’s not your fault.
But it does mean you might have to get creative about where your support comes from.
Find your colleague. Find your people. Find resources that actually speak to what you’re dealing with every day.
Supervision should help you grow. When it doesn’t, build something that will.

Next Week: We’re tackling another brutal truth that keeps clinicians up at night. See you then!
Until Next Week | The Underrated Superhero
© 2025 The Underrated Superhero LLC. All Rights Reserved.
Research Referenced in This Post
- Ellis, M. V., et al. (2014). Inadequate and Harmful Clinical Supervision – Landmark study finding 93% of supervisees receive inadequate supervision and 35.3% receive harmful supervision.
The Counseling Psychologist - SAMHSA TIP 52: Clinical Supervision and Professional Development of the Substance Abuse Counselor – Comprehensive guide on supervision competencies and best practices in SUD treatment settings.
https://store.samhsa.gov - NAADAC Clinical Supervision in the Addiction Profession – Training and resources on supervision best practices specific to addiction counseling.
https://www.naadac.org
Additional Support from The Underrated Superhero
- 📋 Supervision Prep Notepad – Included in the Fall 2025 Survival Kit. Organize your thoughts before supervision so you get something useful out of even imperfect sessions.
- 🎯 New Clinician Survival Kit – Complete toolkit for first-year counselors including the 90-Day Confidence Planner, Quick Capture Cards, and clinical resources.
- 📚 New Clinician Survival Blog Series – All posts in this series covering imposter syndrome, burnout, knowledge gaps, and more.
- 🛠️ Free Clinical Tools – Downloadable resources to support your clinical work. Requires free account.
Previous Posts in the New Clinician Survival Kit Series
- 📖 Am I Documenting Wrong? When Compliance Anxiety Takes Over
- 📖 They Keep Relapsing: When Recovery Doesn’t Look Like You Expected
- 📖 I Don’t Know Enough: When School Didn’t Prepare You for This
See all posts in the New Clinician Survival Kit Series






