Clinical Documentation Overwhelm
I’m looking at my to-do list, and it’s got dozens of progress notes, several assessments, treatment plans that needed to be done yesterday, and I don’t even know how many 60-day reviews. Plus, group notes. Always more group notes.
This wasn’t some unusually bad week. This was just… the job.
When I was carrying 80 clients at an FQHC, the paperwork wasn’t something I did between sessions. It was basically a whole separate position I was also expected to do. And somehow grad school never brought it up.
📚 This is Blog #14 in the New Clinician Survival Kit Series (Click to explore the series)
Weekly honest support for the struggles every clinician faces: “I hate group therapy.” “I can’t do this.” “My client hates me.” “I’m making it worse.” “I can’t say no.” “They’re going to report me.” “I’m too tired to care.” “What do I even say?” “I don’t know enough.” “They keep relapsing.” “Am I documenting wrong?” “My supervisor doesn’t get it.” “I can’t handle this caseload.” “Nobody told me about the paperwork.”
These aren’t signs you’re failing. They’re signs you’re human.
What Grad School Taught Me vs. Clinical Documentation Overwhelm
Look, grad school taught me case conceptualization. The clinical thinking. How to understand what’s going on with a client and connect it to treatment. That part was useful.
What nobody taught me was the actual volume of what I’d be completing every single day.
Admission paperwork. Assessments. Treatment plans due the moment you open a case. Entering clients into the system—which, by the way, has its own whole workflow that nobody explains. Then 60-day reviews. Discharge summaries. Individual notes. Group notes. Case management notes. Six-month insurance and income worksheets. Chart audits.
Times eighty.
And I wasn’t alone. According to SAMHSA’s workforce data, administrative burden is one of the top factors driving clinicians out of the field.

I’m not saying grad school should’ve prepared me for every agency’s specific forms. Every place does things differently, so I don’t know what they realistically could’ve done. But making us actually write sample notes and treatment plans? That would’ve helped. Just some practice with the mechanics of it instead of only the theory.
The Trade-Off
Here’s what I ended up doing, and I’m not saying it was smart: I stopped scheduling time for admin work. I only did documentation when I had no-shows, cancellations, or breaks between sessions.
So, my clinical work stayed protected. Sessions didn’t suffer. But I was working way more hours than anyone should. The paperwork got done—just not during anything resembling normal business hours.
And even then, there were times I had to cancel sessions or call off a couple days of group just to catch up.

That’s the part nobody talks about. The National Council for Mental Wellbeing found that 93% of behavioral health workers report burnout—and paperwork is a major contributor. Either you protect your session time and give up your personal time, or you protect your personal time and fall behind on compliance. I never figured out a version where it all fit neatly into 40 hours. Not with that caseload.
If any of this sounds familiar, you might also relate to “I Can’t Handle This Caseload”—the paperwork problem and the caseload problem feed each other.
Systems That Saved Me from Clinical Documentation Overwhelm
I’m not going to pretend I had some magical solution that made 80 clients feel like 20. It was hard. It was I didn’t make it through 80 clients on determination. I made it through on systems.
Tracking everything in one place.
I built my own workflow spreadsheets that tracked every client’s deadlines—treatment plan due dates, review dates, what signatures were missing. Color-coded so I could glance at it and immediately know what was on fire. Red meant overdue. Yellow meant due soon. Green meant done. Simple, but it kept me from losing track of anything.
The High-Caseload Success Guide walks through this whole system if you want to see how I set it up.
Templates for everything.
Early on I was basically rewriting every note from scratch, which is a ridiculous waste of time. Now I have templates for individual sessions, groups, case management—organized by presenting problems. Templates don’t make your notes generic. They just make the structure automatic so you can focus on what actually matters.
Quick capture tools.
One thing that saved me during sessions was having a simple way to jot down the essentials before I forgot them. The Quick Capture Cards give you a structured format for capturing session details in real time—print them yourself or grab the cardstock version if you want something more durable.
Small rewards for small wins.
This sounds dumb but it worked. I’d reward myself for finishing a few notes—not the whole pile, just a few. Made the mountain feel less impossible.
Batching similar tasks.
Instead of bouncing between clinical thinking and paperwork thinking all day, I’d do all my treatment plan updates in one block, all my progress notes in another. Switching between different types of tasks takes more energy than people realize.
For a deeper dive into documentation systems and efficiency, the Documentation Mastery Sidekick Kit covers these strategies in detail.
What I Wish Someone Had Just Told Me
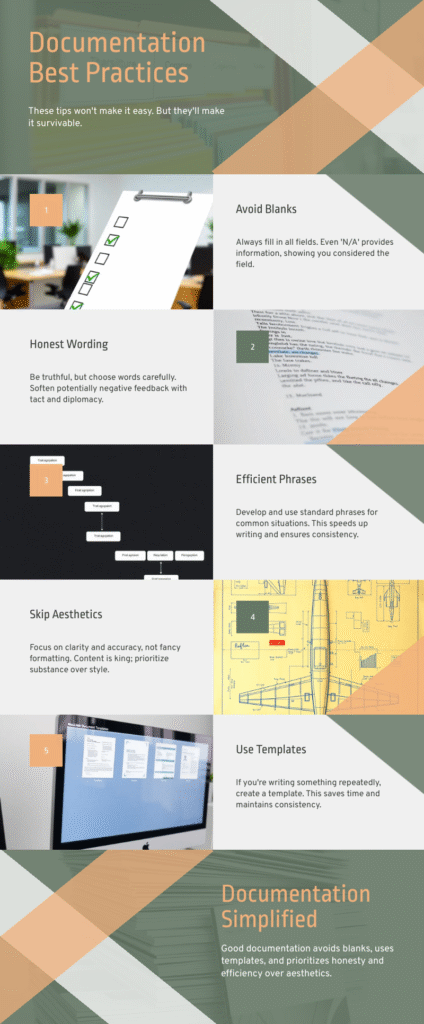
No blanks. Seriously. Before you worry about whether your clinical language is perfect, make sure every field has something in it. Auditors notice blanks.
Be honest but watch your wording. Document what you observe and what the client says. Save your interpretations for treatment planning, not progress notes that could end up in court someday. SAMHSA’s TIP 42 has solid guidelines on documentation standards if you want to dig deeper.
Learn the efficient phrases. “Client denied SI” says the same thing as “Client stated they are not currently experiencing any thoughts of wanting to hurt themselves” but takes way less time. Figure out the short versions that still capture what you need.
Nobody cares if it’s pretty. Clear and compliant beats well-written every time. You’re not being graded on your prose.
If you’re writing the same thing twice, make a template. That’s it. That’s the rule.
If you’re worried about whether your documentation would hold up to scrutiny, I wrote about that fear specifically in “They’re Going to Report Me”.
The Honest Version
Documentation isn’t going anywhere. It’s not getting easier. And agencies aren’t suddenly going to hire enough people to make caseloads reasonable.
So, you can either be mad about it forever, or you can build systems that make it survivable.
I went with systems. Not because I love paperwork—I really, really don’t—but because drowning in documentation was starting to affect how I showed up for clients. And that’s the whole reason I got into this work.
The paperwork is part of the job. Nobody mentioned that in school. But now you know. And you get to decide how you’re going to handle it.
One Thing to Try This Week If You Are Experiencing Clinical Documentation Overwhelm
Pick the documentation task that stresses you out the most—progress notes, treatment plans, tracking compliance, whatever. And build one system for it. A template. A tracking sheet. A blocked-off time on your calendar for batching.
You don’t have to overhaul everything at once. You just have to stop doing it the hard way.

Next Week: We’re tackling another brutal truth that keeps clinicians up at night. See you then!
Until Next Week | The Underrated Superhero
© 2025 The Underrated Superhero LLC. All Rights Reserved.
📖 External Resources & Research
- 🔗 SAMHSA: Behavioral Health Workforce — Federal resources on workforce challenges, including documentation burden and administrative demands on clinicians
- 🔗 PMC Research: Staff Turnover in Substance Abuse Treatment — How administrative burden contributes to annual turnover rates of 19-50% among addiction counselors
- 🔗 National Council: Behavioral Health Workforce Study — 93% of behavioral health workers report burnout; paperwork and administrative tasks cited as major contributing factors
- 🔗 SAMHSA TIP 42: Clinical Documentation Standards — Federal guidelines on documentation requirements for substance use treatment programs
🛠️ Resources from The Underrated Superhero
- 📊 High-Caseload Success Guide — The complete 6-system framework I used to manage 80+ clients, including the color-coded tracking spreadsheets and workflow systems mentioned in this post. Free with membership.
- 📝 Quick Capture Session Cards (PDF) — The 60-second in-session documentation system that keeps notes from piling up. Capture the essentials during session, write the full note later. Free PDF download. | Shop pre-printed cardstock →
- 📂 Clear Documentation Templates Library — Ready-to-use templates for progress notes, treatment plans, and case management documentation so you’re not rewriting from scratch every time.
- 🛠️ The Sidekick: Documentation Mastery Kit (Winter 2026) — Quarterly tools for building sustainable documentation systems, including batch processing strategies and the 6-month Documentation Mastery Planner
- 📧 Subscribe to the New Clinician Survival Kit Series — Weekly honest support for the struggles every clinician faces—no fluff, no toxic positivity
Previous Posts in the New Clinician Survival Kit Series
- 📖 I Can’t Handle This Caseload: When 40 Clients Feels Like 400
- 📖 They’re Going to Report Me: Professional Fear & Compliance Anxiety
- 📖 I Can’t Say No: Setting Boundaries with Clients
See all posts in the New Clinician Survival Kit Series