Therapeutic Alliance with Mandated Clients
Part of the Justice-Involved Treatment Mastery Series

They don’t want to be there. You know it before they even sit down.
Arms crossed. One-word answers. “I don’t have a problem.” Or just… nothing.
And you’re standing there thinking, okay, how exactly am I supposed to help someone who didn’t ask for my help?
I’ve been there. More times than I can count. And what I’ve learned is that you can build a real relationship with mandated clients – but it doesn’t happen the way most of us were trained.
We talked about harm reduction with mandated clients in Blog #1 and working through the tension between court requirements and evidence-based practice in Blog #2. Now we’re getting into the piece that actually makes everything else possible.
Why Therapeutic Alliance with Mandated Clients Matters
I know, I know. “Therapeutic alliance” sounds like something you nod along to in grad school and then forget about when you’ve got 60 clients and paperwork piling up.
But the research is pretty clear – alliance accounts for about 7% of treatment outcomes. That doesn’t sound like much until you realize it’s more than a lot of the specific interventions we stress over.
And with mandated clients? It’s everything. They didn’t choose you. They don’t want to be there. And if you work in community mental health, you know there aren’t a lot of options. This isn’t private practice where clients can shop around until they find the right fit. A lot of times, you’re it. So, the relationship you build – or don’t build – is literally the only thing standing between genuine engagement and someone just running out the clock until their probation ends.
Say What Everyone’s Already Thinking
Here’s something that took me way too long to figure out: when someone walks in hostile, don’t pretend they’re not.
Just say it.
- “You don’t seem like you want to be here.”
- “Sounds like you’re frustrated.”
Nothing fancy. You’re just naming what’s already obvious to both of you.
Why does this work? Because most mandated clients walk in expecting a lecture. They expect you to act like everything’s fine, dive into your intake questions, and pretend you don’t notice they’re glaring at you. When you break that script – when you actually acknowledge what’s happening – it catches them off guard. And that tiny crack? That’s where the work starts.
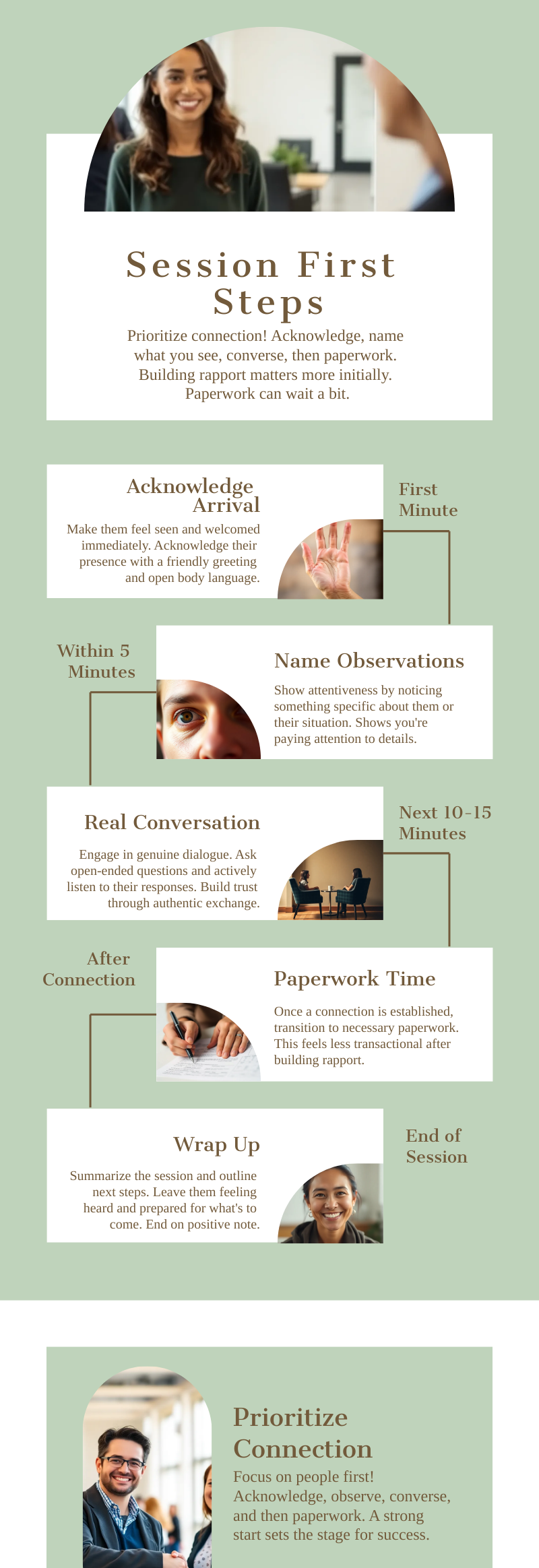
How Paperwork Kills Therapeutic Alliance with Mandated Clients
Can we talk about this for a second? Because I think this is where a lot of newer counselors get stuck.
There’s pressure to get the intake done. Signatures collected. Boxes checked. I get it. But here’s what happens when you shove paperwork at someone who’s already hostile: you get one-word answers, half-blank forms, and a wall that’s twice as high by the time the session ends.
If your agency gives you any flexibility at all, use it. Just talk first. Ask open-ended questions. Let them tell you what happened, what led them here, what they’re frustrated about. Validate what they’re feeling. And honestly? Acknowledge that they showed up. Because they did. They’re sitting in your office right now. That’s not nothing.
Now, I know not everyone has that flexibility. Some agencies want that paperwork done session one, no exceptions. Fine. But even then, you can treat those intake questions like conversation starters instead of a checklist. There’s a difference between “Do you use alcohol?” and “So tell me about your relationship with alcohol – how’d that start?”
They Won’t Believe You When You Say “I Don’t Work for Probation”
You’ll say it. You have to. You’ll explain confidentiality, go over your role, make it clear you’re not reporting back to their PO about every little thing.
And they’ll nod. And they won’t believe you.
Can you blame them? They’ve probably heard this before. Maybe from someone who said it and didn’t mean it. Maybe from someone who meant it but still shared more than they should have.
Here’s what I’ve learned: words don’t build trust with this population. Actions do.
Every time you don’t share something you weren’t required to share. Every time you advocate for them in a staffing or a court report. Every time you treat them like a human being instead of a case file. That’s what actually proves you’re not just another arm of the system.
Research on dual-role relationships backs this up – what works is being caring, fair, and authoritative without being authoritarian. And the quality of this relationship actually predicts outcomes. We’re talking probation violations, revocations, the whole thing.
But I want to be honest with you: some clients will never fully trust you. And that’s okay. You’re not failing if that happens. A lot of these clients have been through treatment before – sometimes multiple times. And not every counselor they’ve worked with was great. Maybe someone broke confidentiality. Maybe someone talked down to them. Maybe someone just didn’t care. They’re carrying all of that into your office. So when they don’t trust you right away, it’s not really about you. Sometimes the best you can do is be consistently trustworthy and let them decide what to do with that.
When Therapeutic Alliance with Mandated Clients Takes Time
So, what happens when you’ve done everything right and they’re still not opening up? Session five. Session ten. Still getting one-word answers and crossed arms.
Do you have a threshold? A point where you decide this isn’t working?
Honestly, I don’t. I just keep showing up. Stay consistent. Let them see that I’m going to be the same person every time they walk in.
That said – I’m not just sitting there waiting. I like a little confrontation. Not aggressive, just… honest. “I’ve noticed you shut down every time we get close to talking about your family. What’s that about?” It shows I’m paying attention. Sometimes that’s what finally cracks things open.
Those Moments When Everything Shifts
Sometimes a client walks in like they want to fight you. “I don’t want to talk. You can’t make me. I’m not going to like this.”
And then something happens. Maybe you said the right thing. Maybe you didn’t say the wrong thing. Maybe they just decided to give you a chance.
By the end of the session, they’re asking when they can come back.
I used to be surprised when this happened. Now I expect it. Not every time, but often enough that I know it’s possible. And when it happens, it’s not luck. It’s what happens when you do your job well and they decide to meet you halfway. Honestly, getting to witness that shift? It’s a gift. That’s the part of this work that keeps you going.
New Counselors and Therapeutic Alliance with Mandated Clients
If you’re early in your career and working with this population, can I tell you something?
You’re going to have sessions that feel like failures. A client’s going to say something harsh. Shut you out completely. Maybe even request a different counselor. And you’re going to walk out of that room wondering if you’re cut out for this work.
Now, I want to be clear – there’s a difference between a hostile client and an abusive one. If a client or a parent is crossing lines, being truly disrespectful or threatening, you don’t just have to sit there and take it. Seek supervision. Request termination if you need to. Setting that boundary isn’t a failure. It’s good clinical practice.
But most of the time? It’s not that. It’s just someone who’s angry and scared and taking it out on whoever’s in front of them.

I still feel that way sometimes. Even after all these years, there’s a part of me that stings when a client goes with someone else. I know all the stuff about good fit and transference and none of it being personal. I know it. But knowing it and feeling it are different things.
Here’s what I want you to hear: their anger isn’t about you. Their resistance isn’t a grade on your performance. They’re walking in with years of history – with the system, with people who were supposed to help, with their own shame. You’re just the person in the room.
Your job isn’t to be perfect. It’s to keep showing up. Be steady. Be the same person every session. That’s what builds trust. Not brilliance. Just consistency.
Something to Try
Next time a mandated client comes in with that “I’d rather be anywhere else” energy:
Name it out loud. Something like “Looks like you’re not thrilled to be here” or “You seem frustrated.” See what happens.
If you can, hold off on the paperwork. Even fifteen minutes of real conversation first can change the whole session.
And when you leave that room after a tough session, remind yourself: their resistance wasn’t about you. But when things go well? You can take a little credit for that.
Month 3 Resources
These are on the Justice-Involved Treatment Mastery Series page:
- Trust-Building Conversation Starters – questions that actually work when someone doesn’t want to talk
- Motivational Interviewing Adaptations for Mandated Clients – MI has solid research showing better attendance, less dropout, lower recidivism. This shows you how to tweak it for this population.
- Resistance vs. Ambivalence Assessment Tool – helps you figure out if they’re actually resistant or just unsure. Changes your whole approach. Download PDF or explore the interactive version below:
Next month: Documentation That Satisfies Courts AND Supports Recovery
References
- Stubbe, D. E. (2018). The therapeutic alliance: The fundamental element of psychotherapy. Focus: The Journal of Lifelong Learning in Psychiatry, 16(4), 402-403. https://pmc.ncbi.nlm.nih.gov/articles/PMC6493237/
- Skeem, J. L., Eno Louden, J., Polaschek, D., & Camp, J. (2007). Assessing relationship quality in mandated community treatment: Blending care with control. Psychological Assessment, 19(4), 397-410. https://pubmed.ncbi.nlm.nih.gov/18085932/
- Gonçalves, L. C., et al. (2025). Effectiveness of motivational interviewing with justice-involved people: A systematic review and meta-analysis. Frontiers in Psychology. https://pmc.ncbi.nlm.nih.gov/articles/PMC12097221/