Filling Therapy Sessions
Fifteen minutes in.
The client is sitting across from me, waiting. I’ve covered intake updates, asked about their week, checked on their sobriety. We’ve done the housekeeping.
And now there are thirty more minutes to fill.
This is the nightmare every new counselor faces: filling therapy sessions when you’ve run out of prepared material. You thought you knew what to talk about. You had your intake questions, your check-ins, your housekeeping. But now you’re staring at the clock and realizing you have no idea how to make this last another half hour.

My heart is racing. I can feel myself starting to blush. The thought loops: I can’t do this. I’m a failure. What am I supposed to talk about?
So, I ask another closed-ended question. The client gives a one-word answer. I jump in too fast, trying to fill the silence, and kill whatever opening might have existed.
Then I do what every panicked new clinician does: I start small talk.
If you’ve ever watched the clock creep from minute 15 to minute 45 wondering what the hell you’re supposed to say for the next half hour, this is for you.
📚 This is Blog #8 in the New Clinician Survival Kit Series (Click to explore the series)
Weekly honest support for the struggles every clinician faces: “I hate group therapy.” “I can’t do this.” “My client hates me.” “I’m making it worse.” “I can’t say no.” “They’re going to report me.” “I’m too tired to care.” “What do I even say?”
These aren’t signs you’re failing. They’re signs you’re human.
Why This Happens (And It’s Not What You Think)
During my first year—both internship and my first job—I was incredibly overwhelmed. The client would be sitting there waiting for me to say something, and I’d be completely done with things to say by 10 to 15 minutes.
And I genuinely believed the problem was that I didn’t know enough about addiction. That I wasn’t smart enough or didn’t have enough training.
But that wasn’t it.
I was relying on announcements and housekeeping to guide the session. That was my strategy for filling therapy sessions—except it wasn’t therapy at all.
I’d come in with program updates, group schedule changes, reminders about documentation, check-ins about their week. And when that ran out at the 10-15 minute mark, I had nothing. Because I wasn’t actually doing therapy. I was doing administration with occasional therapeutic questions sprinkled in, and when that ran out, I had no strategy for filling therapy sessions with actual therapeutic content.
When I did ask open-ended questions—the kind that were supposed to spark more discussion—I panicked at the first sign of resistance. Client paused to think? I jumped in. Client gave a short answer? I moved on. Client looked uncomfortable? I changed the subject.
Definitely amateur hour.
The Real Challenge of Filling Therapy Sessions
I had discussions with my supervisor. “What am I supposed to talk about for these sessions?…”
She had advice and suggestions—good ones, probably. Ask about their family. Explore their trauma. Use motivational interviewing.
But it didn’t help. Because the problem wasn’t what to ask. The problem was how I was asking those questions. My delivery was quick, closed-ended. Or if I did manage to ask something open-ended, I responded too soon and ended that golden moment before it could breathe.
That’s what connects to what we talked about in “I Can’t Say No”—sometimes the problem isn’t the technique. It’s our discomfort with letting things unfold naturally.
What Doesn’t Work When Filling Therapy Sessions
I can’t really remember the panic anymore because I don’t do it now. I love sessions and generally don’t find myself looking at the clock unless the client is very quiet and I’m grasping at straws due to little to no verbal and nonverbal communication.
But before? My heart would beat faster. I would start thinking, “I can’t do this.” “I’m a failure.” And I’m sure I would blush—I blush when I’m anxious.
So, what did I do? I panicked and tried everything.
Automated Check-Ins
In the past when I was struggling, I would do automated check-ins with everyone—going around the room or through my individual caseload doing surface-level questions, hoping that through this I would find openings in their responses for open-ended questions that would further provoke processing.
“How’s your week?” “Any cravings?” “Sleep okay?” “Family doing alright?”
Just hoping, praying that someone would say something—anything—that gave me material to work with.
Sometimes it worked. Most times it didn’t.
Small Talk
And then of course there are those dreaded fillers that nervous people do in conversations. The dreaded small talk.
Weather. Weekend plans. Their kid’s soccer game. Anything to avoid the terrifying quiet.
It felt better than silence. But I knew—I knew—it wasn’t therapy.
The Uncomfortable Truth About Silence
Here’s what’s so important about silence in sessions: There are different kinds, and you have to learn to sit with both.
Productive Silence
Productive silence is generally seen as times of silence when you’re letting the client sit with difficult feelings or reflective thoughts. You should let this breathe. It’s therapeutic.
You’ll know it’s productive silence when the client looks thoughtful, not uncomfortable. They’re processing, not waiting for you to rescue them. The silence has weight—it feels purposeful.
But then there are other silences. The ones where you’re flailing because you genuinely don’t know what to say next.
And honestly? Those silences are still important. Even if you feel like you’re flailing, generally the client will fill those gaps. And what they say—or don’t say—is very telling. Their body language. Their facial expressions. Whether they jump in to fill the silence or sit comfortably with it. Whether they change the subject or lean into discomfort.
All of that is therapeutic data.
But I’m still not all that good at those moments. I have to take a drink or fiddle with my hands to keep from talking. Because silence feels like failure. It feels like I should be doing something.
The concept of “therapeutic silence” is well-documented in counseling literature. Research from the American Counseling Association shows that pauses in conversation allow clients to process emotions and arrive at their own insights—something we often rush past in our discomfort.

What Actually Changed
I didn’t suddenly get better at asking questions or managing awkward silences.
What changed was I absorbed more information about substance abuse and addictions. Just time and experience.
Before, I was fearful about being seen as knowledgeable and professional. So I stuck to safe, surface-level questions because I was terrified of being exposed as incompetent.
But as I gained experience—more sessions, more clients, more situations I’d already navigated—I grew more comfortable with impromptu sessions or questions that clients would ask.
A client would ask a random question about withdrawal or MAT or whether their drinking “counted” as a relapse, and instead of panicking, I’d think: Oh, I know this. Let’s talk about it.
Then I started welcoming those moments instead of fearing them.

Because once I had a foundation of knowledge, I didn't need a script. I could follow the client's lead. That's when filling therapy sessions stopped feeling like a performance I had to execute perfectly. Instead, it became a conversation I could navigate with confidence—even when I didn't know exactly where it was going.
This shift from fear to confidence is what we explored in "I Can't Do This" - competence comes from experience, not from knowing everything on day one.It Still Happens (And That’s Okay)
Even now, years into this work, I will tell you that I have had sessions where I’m unsure that we accomplished anything at all. Fearing that it was either all superficial conversation, possibly bordering on solution-focused therapy or relapse prevention but barely.
Sessions that felt pointless.
And then the client comes back the next week and says: “That session was really helpful.”
So, I don’t know. Maybe what feels aimless to me is exactly what they needed. Like we discussed in “I’m Making It Worse”, sometimes what feels ineffective to us is actually exactly what the client needs.
Even when clients were happy, I used to just sit there wondering if I’d actually done anything therapeutic.
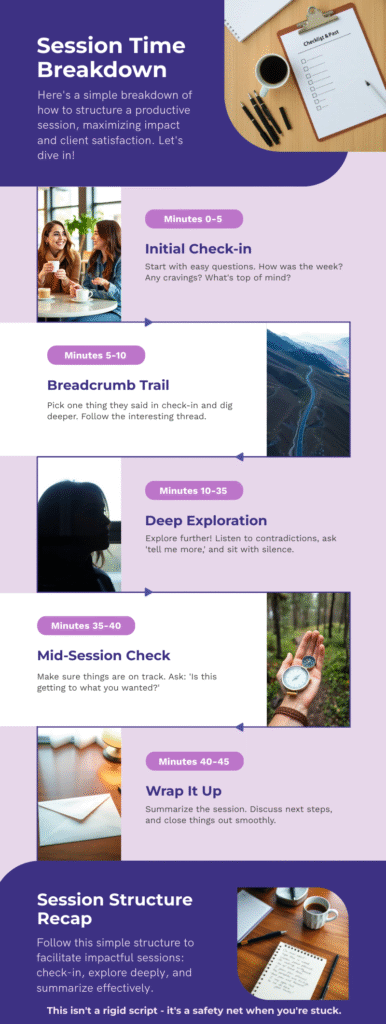
Now? I’m much more comfortable saying mid-session: “Is this getting to what you wanted to accomplish this session. Or as we continue, would you like to explore anything else as a priority?”

Sometimes the client says, “Yeah, this is good.” And I relax, trusting that what feels aimless to me might be exactly what they need.
Sometimes they say, “Actually, I wanted to talk about…” And we pivot.
Either way, I’m not sitting there panicking anymore. I’m just checking in.
Practical Tools for Filling Therapy Sessions

Alright. Enough about what doesn’t work. Let me tell you what actually does—or at least what’s helped me.
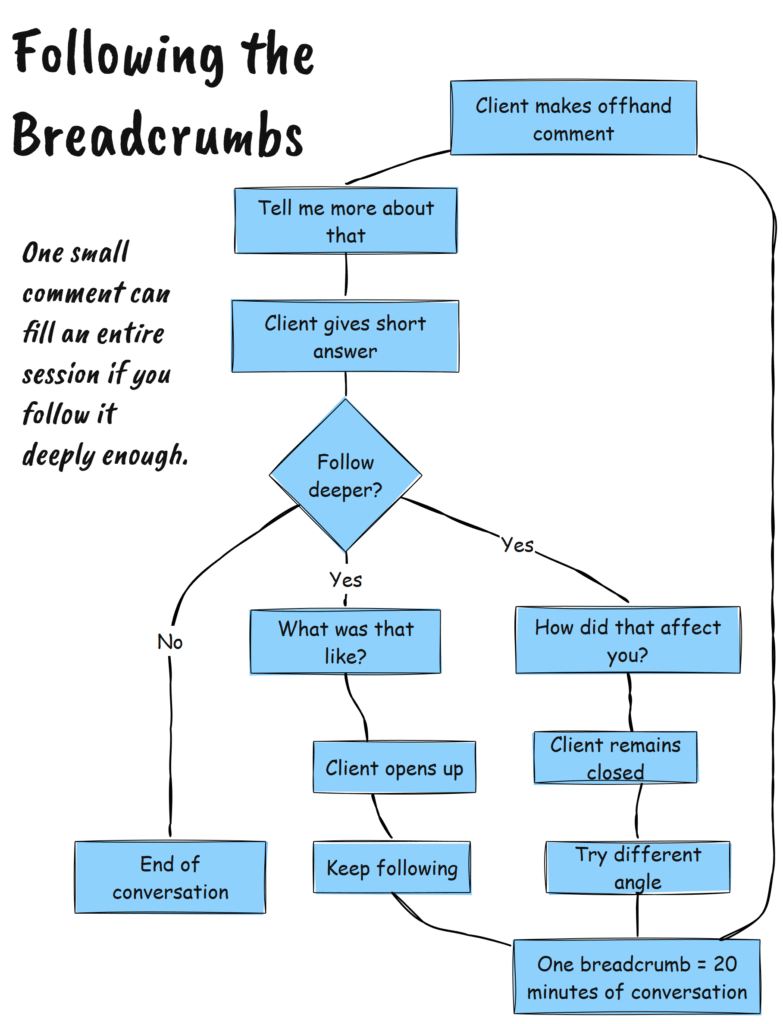
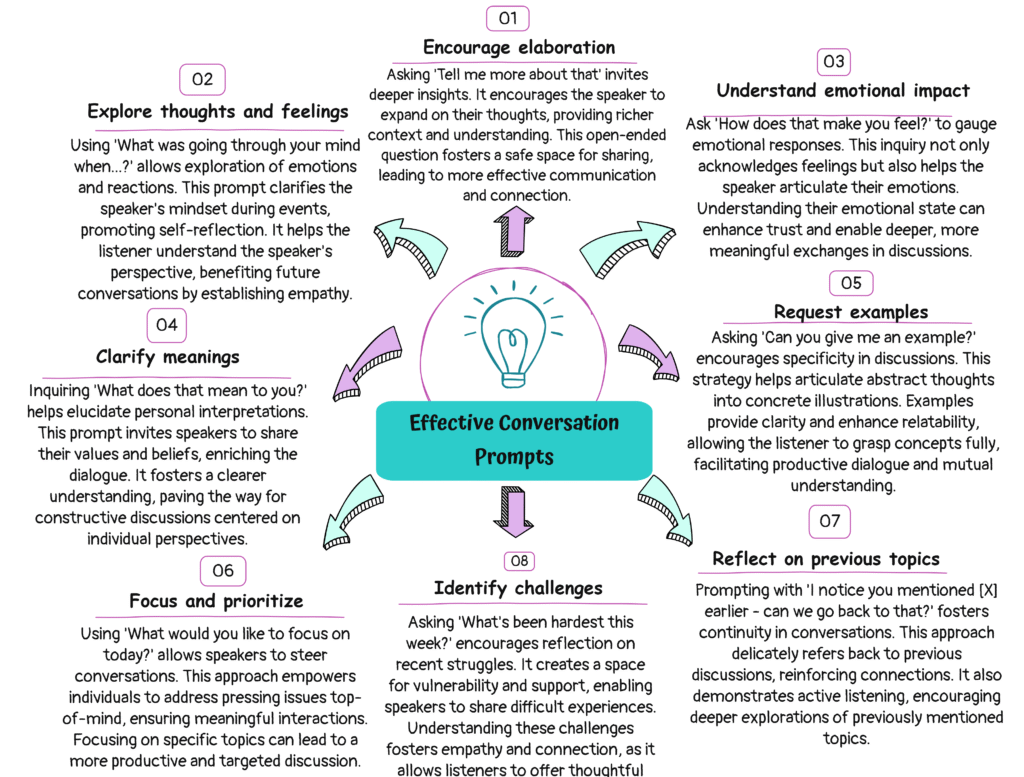
Follow the Breadcrumbs
Clients drop breadcrumbs constantly. Small comments that hint at bigger issues.
“I’ve been sleeping weird lately.”
“My mom called again.”
“Work’s been stressful.”
Most of the time, we just move on. We acknowledge it and ask the next question on our mental checklist.
But what if you didn’t move on? What if you followed the breadcrumb?
“Sleeping weird how? What’s different?”
“What happened when your mom called?”
“Tell me more about the work stress.”
One breadcrumb can fill 20 minutes if you follow it deeply enough. I’m not kidding. One offhand comment about sleep can turn into a conversation about nightmares, which leads to trauma, which leads to using as a coping mechanism, which leads to their relationship with their partner who doesn’t understand why they can’t just “get over it.”
You just have to follow it.
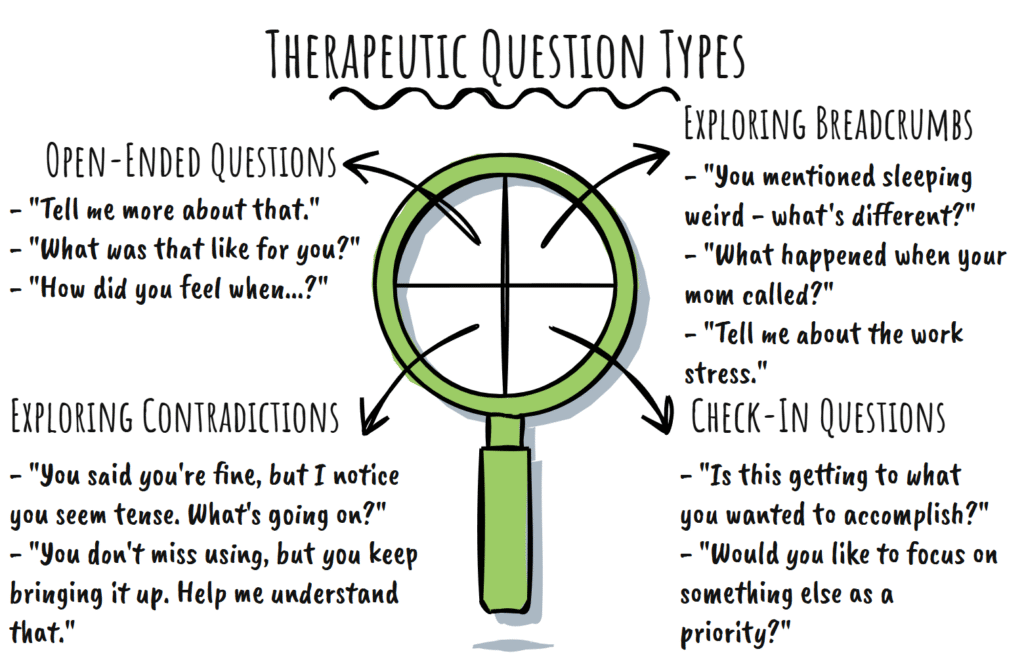
“Tell Me More About That”
When a client gives a short answer, resist the urge to jump to the next question.
Instead, just say: “Tell me more about that.”
That’s it. That’s the whole technique.
You’d be surprised—or maybe you wouldn’t be—how much clients will say if you just give them space to expand instead of rushing to fill the silence.
Notice the Contradictions
Clients contradict themselves all the time.
“I’m fine.” (But their body language says otherwise.)
“I don’t miss using.” (But they keep talking about it.)
“My family’s supportive.” (But they won’t call them.)
When you notice a contradiction, name it. Gently.
“You said you’re fine, but I notice you seem tense. What’s going on?”
This is rooted in motivational interviewing principles. SAMHSA’s guide to MI emphasizes reflective listening and exploring ambivalence—both of which require sitting with contradiction.
This opens up real conversations. Not surface-level check-ins. Real stuff.

Get Comfortable with “I Don’t Know”
If you’re in productive silence and you’re struggling not to talk, try this: take a sip of water. Shift in your seat. Look at your notes.
Physical actions that keep your mouth busy so you don’t interrupt the client’s processing.
And if the silence goes too long and you genuinely don’t know what to say?
Say that.
“I’m sitting with what you just shared. Give me a second to think about where to go next.”
I think—and I could be wrong—but I think clients trust you more when you’re honest about not knowing everything. At least, that’s been my experience.
Client asks you a question you don’t know the answer to? Don’t make something up. Don’t deflect.
Say: “I don’t know. Let’s figure it out together.” Or: “That’s a great question. Let me look into that and we can talk about it next session.”
You’re not supposed to know everything. And pretending you do just makes you look like you’re trying too hard.
The Truth About Filling Therapy Sessions
I wish someone had told me this in year one: the problem isn’t that you don’t know what to say. The problem is that you’re uncomfortable with not knowing.
You think sessions should flow smoothly. You think you should always have the next question ready. You think silence means you’re failing.
But therapy isn’t a performance. It’s a process. And filling therapy sessions isn’t about having brilliant insights for 45 straight minutes—it’s about creating space for the client to process, explore, and discover.
Some sessions will feel aimless. Some clients will give you nothing to work with. Some silences will be uncomfortable.
And that’s okay.
The National Institute on Drug Abuse notes that effective therapy isn’t about rigid adherence to scripts—it’s about building rapport and meeting clients where they are.
The more comfortable you get with discomfort, the better clinician you become.
You stop filling time with small talk. You stop killing golden moments by jumping in too fast. You stop panicking when there are 30 minutes left and no clear direction.
You start trusting the process.

Final Thoughts
I still fidget during silence. I still have sessions where I walk away wondering if we accomplished anything. I still occasionally glance at the clock and think, How are there still 15 minutes left?
But I don’t panic anymore.
Because I know now that therapy isn’t about filling 45 minutes with brilliant insights.
It’s about showing up, following the client’s lead, and trusting that even the aimless-feeling sessions are doing something.
You don’t need to know what to say every second of every session.
You just need to be comfortable enough to sit in the not-knowing until the next moment reveals itself.
Tools for This Week
Try This: Next session, when you ask an open-ended question, count to 10 before you say anything else. Let the client sit with it. See what happens.
Reflection Prompt:
Think about your last “aimless” session. What breadcrumbs did the client drop that you didn’t follow? Write them down. Practice noticing them in real time.
Resource:
Download the Session Conversation Starters from our free tools and resources — prompts that open real conversations, not surface-level check-ins.
Next Week: We’re tackling another brutal truth that keeps clinicians up at night. See you then!
Until Next Week | The Underrated Superhero
© 2025 The Underrated Superhero LLC. All Rights Reserved.
Resources Referenced in This Post
- American Counseling Association (ACA) – Research and resources on therapeutic silence, active listening, and creating space for client processing
https://www.counseling.org - SAMHSA’s Guide to Motivational Interviewing – Evidence-based techniques for reflective listening, exploring ambivalence, and asking open-ended questions that deepen therapeutic conversations
https://www.samhsa.gov/brss-tacs/recovery-support-tools/motivational-interviewing - National Institute on Drug Abuse (NIDA): Principles of Drug Addiction Treatment – Research on effective therapy approaches, building rapport, and meeting clients where they are rather than following rigid scripts
https://nida.nih.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/evidence-based-approaches-to-drug-addiction-treatment/behavioral-therapies
Additional Support from The Underrated Superhero
- 📚 Quick Capture Progress Note System – Streamline documentation so you can spend less time on notes and more time focusing on what actually happens in sessions
- 🛠️ New Clinician Survival Kit – Quarterly tools including Session Conversation Starters, Clinical Confidence Frameworks, and strategies for navigating difficult therapeutic moments
- 📝 Free Clinical Tools – Download the free Conversation Starter Guide for Substance Use Screening—a visual flowchart with scripts and prompts that help you open respectful, stigma-free conversations in any setting. Requires free account.
- 📧 Subscribe to the New Clinician Survival Kit Series – Weekly honest support for the struggles every clinician faces—no fluff, no toxic positivity, just real talk
Want More Conversation Frameworks?
Premium and All-Inclusive members get access to advanced conversation tools and therapeutic frameworks:
- 💬 How to Talk About Substance Use (PNG and PDF) – Clinician-facing guide with scripts, prompts, and conversation techniques for discussing substance use without stigma or shame. Covers motivational interviewing elements and recovery-oriented language. (Premium members)
- 🗣️ Quick Guide: Conversation Starters and Language Shifts for Resistance in High Functioning Clients – Targeted strategies for navigating resistance, ambivalence, and deflection with clients who appear “fine” on the surface. (Premium members)
- ⚡ Tough Conversations and Sticky Situations (PDF) – Comprehensive framework for handling difficult therapeutic moments, boundary violations, and conversations that make you uncomfortable. (All-Inclusive members)
Previous posts in the New Clinician Survival Kit Series:
Week 1: I Hate Group Therapy: How I Went from Dreading sessions to Loving Them
Week 2: I Can’t Do This: When Imposter Syndrome for Therapists Hits Hardest
Week 3: My Client Hates Me: When Resistance Feels Personal
Week 4: I’m Making It Worse: Fear of Harming Clients
Week 5: I Can’t Say No: Setting Boundaries with Clients
Week 6: They’re Going to Report Me: Professional Fear & Compliance Anxiety
Week 7: I’m Too Tired to Care: Burnout and Compassion Fatigue






