Blog #2 in the Justice-Involved Treatment Mastery Series: Harm Reduction with Court-Mandated Clients
Read Blog #1: Beyond Court Compliance if you haven’t already.
The email from probation hits your inbox: “How many more passes are we going to give this client?”
Your client is still using. You know it. Probation knows it. The court knows it.
But here’s what that email doesn’t capture: Your client has shown up to every single session for three months. They’re participating. They’re working on employment. They’re rebuilding relationships with their kids. They’re doing the work.
Just not the abstinence part. Not yet.
And now probation wants to know when you’re going to “hold them accountable” with a violation or bump them up to residential.
So what do you do when the court orders abstinence but your client needs harm reduction?
This is the daily tension you navigate as a counselor working with mandated clients. Practicing harm reduction with court-mandated clients isn’t about choosing between compliance and evidence-based care—it’s about understanding how to integrate both effectively.
You learn that by actually working with people. And by realizing pretty quickly that “telling on them” to probation isn’t always what’s best for their recovery—even when you’re required to report. Before you can practice harm reduction effectively, though, there’s a crucial first step most counselors overlook.
Building Trust Takes Time (And Probation Officers Are Watching You Too)
The Testing Phase: “How Many More Passes?”
Here’s what I learned over the years: probation officers don’t automatically trust your clinical judgment. Especially when you’re new.
When they first meet you, they’re cautious. They push back—not aggressively, just… testing. Passive statements in emails. “We’re giving them another pass?” or “When are we going to hold them accountable?”
What they’re really asking is: Are you going to let this client slide forever, or do you actually know what you’re doing?
Because they’ve seen plenty of counselors who either:
- Over-report everything and create unnecessary violations, or
- Under-report and hide problems until they explode
So they’re watching to see which kind of counselor YOU are. However, this testing phase doesn’t last forever. Here’s how the dynamic shift.
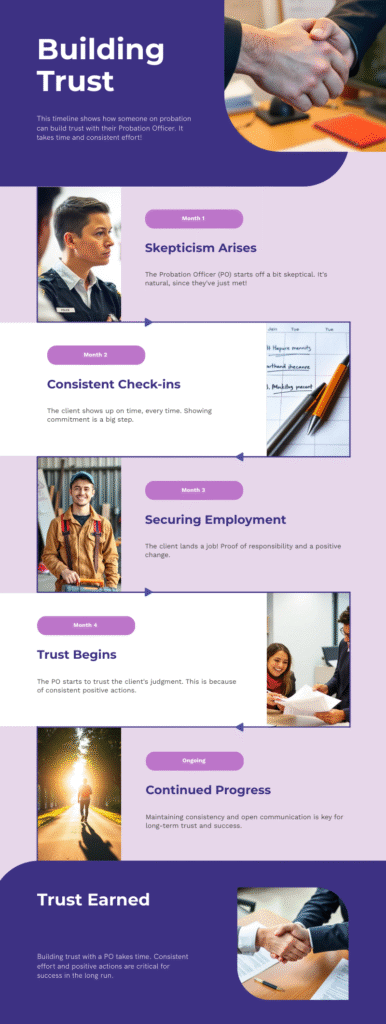
How the Shift Happens
The shift happens gradually. You advocate for your client staying at your program. Probation is skeptical. Then a month later, they see the client is still showing up. Two months later, the client gets a job. Three months in, the client is reconnecting with family.
And suddenly that probation officer isn’t questioning your judgment anymore. They start trusting that you know what you’re doing. But earning trust isn’t just about client progress. There’s another critical component.
Demonstrating Accountability
Importantly, you also have to show probation that you’re NOT just holding onto clients who need a higher level of care. You have to demonstrate accountability too.
When it’s genuinely not working? When your client isn’t showing up, isn’t engaging, is escalating in their use? You have to be honest about that. You have to recommend that higher level of care even when you don’t want to lose the client.
That’s how you build credibility. Probation officers need to see that you’re balancing clinical support with realistic assessment. You’re not just an advocate—you’re a professional who can tell the difference between “client is struggling but progressing” and “client needs more intensive services.”
Once they trust you, everything changes. Those questioning emails stop. They start calling YOU for recommendations instead of dictating them. They actually listen when you say “This client is making progress even though they’re still using.”
But you have to earn that trust. And it takes time.
Research confirms this: building therapeutic alliance while incorporating procedural justice principles is more effective at reducing recidivism than surveillance and punishment approaches. This is exactly why harm reduction with court-mandated clients requires a long-term relationship-building strategy, not just compliance monitoring.
Once you’ve established that trust, you can start reframing conversations with the court. Because here’s what most counselors misunderstand:
What Courts Actually Want (Hint: It’s Not Punishment)

When I advocate for a client to stay at our program—despite continued substance use—I’m not ignoring what the court wants. I’m actually delivering on what they’re asking for.
Think about it: What does the judge actually want when they mandate treatment?
- Reduced recidivism
- Community safety
- Client stability
- Treatment engagement
They want outcomes. And sometimes, harm reduction delivers those outcomes better than abstinence-only approaches.
The Battle I Fight Constantly
Let me give you a concrete example of how I frame this. I’ve fought this battle so many times. Client is still using. Probation wants residential. Court is talking violations. And I’m sitting there saying, “But look at what IS happening.”
This client has shown up consistently for three months—that’s the longest period of treatment engagement in their entire history. They’re working on housing. They got a job. They’re rebuilding relationships with their kids. They haven’t picked up new charges.
Yes, they’re still using substances. But they’re also building a life that supports recovery. They’re creating protective factors. They’re developing skills.
You know what happens when you yank them out of that progress and throw them into residential treatment? Half the time, they don’t complete it. They run. They disengage completely. And then they’re back in front of the judge with new charges and zero treatment progress.
How I Frame Harm Reduction with Court-Mandated Clients for Court
So when I advocate for them to stay, I frame it around what the court actually needs to see:
“This client has demonstrated 100% attendance for three months. They’re working toward employment and housing stability. They’re engaged in treatment and building recovery skills. Moving them to a higher level of care right now risks disrupting real progress that’s working.”
Sometimes I win that battle. Sometimes I don’t.
But every single time, I make sure the court understands: You want compliance or you want outcomes. Pick one. Because rigid abstinence mandates often get you neither. So how do you actually implement this in practice? Let’s break it down into five concrete strategies.
What Harm Reduction with Court-Mandated Clients Actually Looks Like
Let’s get specific. Because “harm reduction with court-mandated clients” sounds abstract until you see what it actually means in practice.
1. Front-Loading Relapse Prevention
Most programs wait until someone relapses, then respond. That’s backwards.
Instead: Build the safety plan BEFORE crisis hits.
In early sessions, I’m already asking: “What situations make you most likely to use? Who can you call when cravings hit? What’s your backup plan if your first strategy doesn’t work?”
We’re not planning FOR them to relapse. We’re planning for what happens IF they feel close to using, so we can prevent both the use AND the legal consequences.
Document it as “relapse prevention planning” and you’re good. Because that’s exactly what it is. But front-loading prevention only works if clients feel safe being honest with you. Which brings us to the second essential strategy.
2. Creating Safety for Honesty
The Conversation That Changes Everything
Here’s a conversation I have regularly with mandated clients—usually in the first few sessions:
Client: “What happens if I use? Do I have to tell you?”
Me: “Here’s the truth: I need you to be honest with me. Because your drug test results are definitely getting sent to probation. So if you’re going to test positive, tell me NOW. Before the test comes back. Because if you tell me now, we can work together on how to handle this and what we’re going to do about it.”
What “Working Together” Actually Means
And then I explain what I mean by “what we’re going to do about it”:
- We’ll talk about whether YOU want to tell your probation officer yourself (which usually goes better than them finding out from a lab result)
- We’ll come up with a plan—what goals you’re willing to work on because of the relapse, what supports you need, what’s going to be different this week
- I’ll be there with you for that conversation if you need me, or we’ll write it out together
- Sometimes we’ll call the probation officer together, right from my office, with you on the line
The point is: we go in with a plan. Things always come out better when there’s a plan in place.
I also tell them this: “Drug tests can be empowering tools to show when you ARE testing negative. Let’s use them that way instead of just as gotcha moments.”
This is harm reduction with court-mandated clients in action.
I’m not saying “lie to probation.” I’m not hiding substance use. I’m creating a space where clients can be honest BEFORE crisis hits, so we can reduce both the harm AND the legal consequences.
The Result: Proactive Help-Seeking
And you know what happens when clients know they can be honest with you?
They start reaching out BEFORE they use. They call you when cravings hit. They bring situations to you proactively instead of hiding until everything falls apart.
That’s when real harm reduction happens—in the space between craving and use, in the moment when someone reaches out instead of isolates.
And that only works if they trust you. Which only happens if you’ve created actual safety for honesty. Beyond creating safety for disclosure, there’s another harm reduction strategy that’s often misunderstood by courts.
3. Medication-Assisted Treatment: When I Realized Not Everyone Gets It
When I Realized Not Everyone Gets It
I was lucky early in my career. I worked in a program that understood MAT. We had clients on methadone, buprenorphine, naltrexone. Everyone—clinical staff, supervisors, even most of the probation officers we worked with—recognized it as evidence-based treatment, not “replacing one drug with another.”
So I got to see MAT work. I watched clients stabilize. I saw overdose risk drop. I saw people rebuild their lives while on medication.
It wasn’t until I started working with clients in the jail system that I realized: not everyone sees it this way.
The Jail System Wake-Up Call
Clients would come in and tell me their meds were withheld. They went through withdrawal. They experienced unnecessary hardship. And when they were released, they were at massively increased risk for overdose because their tolerance had dropped.
I couldn’t advocate directly to the jail in most cases—the system just didn’t work that way. But I could document the hell out of what was happening and advocate on every other front: connecting clients with MAT providers immediately upon release, educating probation officers about overdose risk, pushing back when courts treated MAT as non-compliance with “abstinence.”
MAT is harm reduction. Full stop.
If your client is on medication for opioid use disorder, you’re already practicing harm reduction with court-mandated clients within the bounds of judicial requirements. And if you’re in a jurisdiction that doesn’t accept MAT as legitimate treatment? You’ve got evidence-based advocacy work to do.
Because the research is clear: MAT reduces overdose deaths by about 50%, reduces criminal recidivism, and improves treatment retention compared to abstinence-only approaches.
Your documentation language matters:
- “Client is engaging in FDA-approved medication for opioid use disorder as part of evidence-based treatment plan”
- “MAT supports client’s recovery goals and significantly reduces mortality risk”
- “Client demonstrates medication compliance and active participation in treatment”
Frame it as what it is: medical treatment for a medical condition. Even with MAT and safety planning in place, you’ll still need a framework for responding when clients use. That’s where graduated responses come in.
4. Graduated Responses (Not Everything Is a Violation)
Abstinence-only thinking treats everything the same: Use = failure = report to court = sanctions.
That’s not how change works.
Build a continuum of responses into your treatment plan from day one:
- Client reports cravings or high-risk situations? Increase support, adjust treatment plan. That’s clinical response, not court notification.
- Client uses once but self-reports and stays engaged? That might warrant court notification WITH a treatment plan adjustment, but the focus is on safety and continued engagement.
- Client uses repeatedly and stops coming to treatment? Now you’re talking clinical and court response, reassessment of level of care.
The point is: you’re responding to the CLIENT’S SAFETY and ENGAGEMENT, not just checking boxes for compliance.
And yeah, sometimes you still have to report use to probation. But you can frame it as part of ongoing treatment engagement rather than evidence of failure. The strategy that causes the most anxiety for new counselors—but is arguably the most important is as follows.

5. Harm Reduction Saves Lives (And I’m Not Uncomfortable Saying That)
Some counselors get nervous about documenting harm reduction strategies. They worry it looks like they’re “encouraging use.”
I don’t have that problem. Harm reduction with court-mandated clients saves lives, and I voice that all the time.
I worked closely with the harm reduction program—they’re the ones distributing naloxone, doing outreach, connecting with people who use drugs. They’ve saved hundreds of lives. Literally hundreds.
If your client is going to use despite your best clinical efforts, wouldn’t you rather they survive that use?
You can simultaneously:
- Support abstinence goals
- Teach harm reduction strategies
- Keep your client alive
Those aren’t contradictory. They’re complementary.
How to document this:
“Client educated on overdose prevention strategies including: not using alone, starting with smaller amounts after periods of abstinence, having naloxone available, and recognizing signs requiring immediate medical attention. Client verbalized understanding that these strategies are risk reduction education, not endorsement of substance use, and are provided to reduce mortality risk if relapse occurs.”
You’re not encouraging use. You’re preventing death. This aligns with SAMHSA’s harm reduction framework, which emphasizes meeting people where they are and reducing the negative consequences of substance use.
And if anyone questions that? You can point to the evidence. You can point to the lives saved. You can ask them directly: “Would you rather this client died from an overdose that could have been prevented?”
There’s nothing uncomfortable about keeping people alive. Now let’s talk about the moment that terrifies most counselors—when theory meets reality.
The Documentation Dance: How to Write About This
Your clinical notes need to do three things simultaneously:
- Demonstrate treatment compliance
- Reflect evidence-based practice
- Protect your client
This is where the Abstinence vs. Harm Reduction Treatment Goal Translator becomes essential. It’s the tool that helps you write treatment goals the court will accept while implementing the harm reduction strategies your client actually needs.
Abstinence vs. Harm Reduction Treatment Goal Translator
This is where the Abstinence vs. Harm Reduction Treatment Goal Translator becomes essential. It’s the tool that helps you write treatment goals the court will accept while implementing the harm reduction strategies your client actually needs.
What’s Inside: 20+ side-by-side examples across 5 categories (Substance Use Goals, Attendance Goals, Safety Goals, Accountability Goals, Life Stability Goals) showing exactly how to translate abstinence language into court-friendly harm reduction goals.
Sample: Substance Use & Recovery Goals
| Court/Abstinence Language | Evidence-Based Harm Reduction | Court-Friendly Phrasing |
|---|---|---|
| Client will achieve complete abstinence from all substances | Client will progressively reduce substance use and associated risks | Client will demonstrate progressive risk reduction with zero legal complications and measurable improvements in stability |
| Client will test negative for all substances | Client will engage in regular monitoring and demonstrate treatment participation | Client will maintain compliance with all court-required monitoring and demonstrate consistent treatment engagement |
The full resource includes 20+ examples across 5 goal categories with detailed documentation tips.
Language that works:
- ❌ Don’t write: “Client agrees to abstinence”
- ✅ Do write: “Client identifies abstinence as primary goal; treatment plan includes progressive intervention strategies to support this goal and reduce harm”
- ❌ Don’t write: “Client used substances, violating treatment contract”
- ✅ Do write: “Client reported substance use on [date]; remained engaged in treatment, self-disclosed use, and participated in safety planning and treatment plan adjustment”
- ❌ Don’t write: “Provided harm reduction education”
- ✅ Do write: “Provided evidence-based relapse prevention education including risk reduction strategies and overdose prevention, consistent with SAMHSA guidelines for SUD treatment”
See the difference? You’re documenting the exact same clinical work, but you’re framing it in language that demonstrates treatment engagement and evidence-based practice. One of the most challenging aspects of harm reduction with court-mandated clients is navigating moments of crisis and disclosure. Here’s how to handle the conversation that keeps counselors up at night.
When a Client Tells You They Used
Your Response Matters Most
Your mandated client walks in and says, “I used this weekend.”
This is the moment that defines everything.
If your response is immediate panic, punishment language, or “I have to report this to your PO right now”—you’ve just taught them never to be honest with you again.
The Six-Step Framework
Instead, here’s what actually works:
- Thank them. “I’m glad you told me. That took guts.”
- Check safety. “Are you okay right now? Do you need medical attention?”
- Understand what happened. “What was going on before you used?”
- Problem-solve together. “What do you think would help prevent this next time? What was missing?”
- Be transparent. “Here’s what I’m required to report and how we’ll document this.”
- Plan next steps. “Let’s figure out how to strengthen your supports this week.”
No shame. No threats. Just honest problem-solving.
And then document it using the “Yes, And” framework: Client self-reported use AND remained engaged in treatment. Client participated in safety planning AND identified specific triggers. Client demonstrates continued commitment to treatment goals AND realistic engagement with recovery.
You’re documenting both the use AND the engagement. Because both are true. This dual documentation approach is formalized in what I call the “Yes, And” framework.

The “Yes, And” Framework: Document Both Realities
Traditional progress notes for mandated clients feel like you’re writing two different stories: the “official” court version and the “real” clinical version.
This is where harm reduction with court-mandated clients becomes visible in your documentation—you stop choosing between court language and clinical reality. Document both in the same note.
Structure your notes in three parts:
Court Compliance: Attendance, drug test results, requirement adherence
Clinical Progress: Harm reduction milestones, safety improvements, skills being developed
Risk & Safety: Current risks, protective factors, crisis plan, next steps
This lets you write notes like:
“Client attended 4/4 sessions this week AND self-reported weekend use. Client engaged in safety planning, identified triggers (argument with partner, missed support meeting) AND developed concrete strategies to strengthen protective factors. Client demonstrates continued treatment commitment AND realistic engagement with relapse prevention.”
You’re being honest about the use. You’re also being honest about the engagement, the progress, the work being done.
Both things are true. Document both. Of course, documenting effectively doesn’t help if you freeze when clients ask the hard questions. Let’s address those now in this next section.
The “Yes, And” Progress Note Framework
Stop writing two different narratives. The “Yes, And” Progress Note Framework is a structured template that lets you document court compliance AND clinical progress in a single, integrated note. Use it as a reference guide when typing notes, or print it out to fill in by hand during sessions.
What’s Inside: 3-section template (Court Compliance Status, Clinical Progress, Risk Assessment & Management) with detailed examples for each section, plus 3 complete sample notes for common scenarios like self-reported use and ongoing progress despite continued substance use.
Sample: Client Self-Reports Weekend Use
Client attended 4/4 sessions this week (100% attendance) AND self-reported weekend substance use on Saturday night. Client tested positive for cocaine on Monday UA AND remained engaged in treatment, participating immediately in safety planning session.
Client identified specific triggers that preceded use (argument with partner Friday evening, missed support meeting Saturday morning) AND developed concrete strategies to strengthen protective factors this week including scheduling daily check-in texts with sponsor and attending 3 meetings minimum.
✓ Court sees: 100% attendance, proactive engagement, safety planning
✓ Clinical reality: Honest disclosure, treatment alliance intact, risk reduction
The full framework includes 3 complete sample notes and a structured template to guide your documentation.
I Got Tired of Writing Letters (So I Created Something Better)
The Monthly Reporting Struggle
Here’s what used to happen: Every month, I’d need to send probation an update on my mandated clients. And every month, I’d sit there staring at a blank document, trying to figure out what to write.
How much do I share? How do I frame this client’s progress? What if I say too much and it gets used against them? What if I say too little and probation thinks I’m hiding something?
It was time-consuming. I was avoiding it. And honestly? Probation would often reach out to me asking for updates because I hadn’t sent them anything, and I really didn’t want them to feel like they had to chase me down.
Creating a System I Could Commit To
I needed something I could commit to. Something regular that wouldn’t need reminding.
So, I created a standardized form system specifically designed for harm reduction with court-mandated clients—one that protects both clinical work and the therapeutic relationship.
Three simple forms that give probation exactly what they need while protecting my clinical work and my clients:
- Admission Form – sent when clients start treatment
- Monthly Progress Form – sent regularly during treatment
- Discharge Form – sent when clients complete or leave treatment
Each form captures the essentials: demographics, services provided, attendance, drug test results, treatment goals, participation summary. That’s it. No detailed session content. No clinical formulations. Just the data points probation officers actually need.
Why This System Works (When Letter-Writing Doesn’t)
The Problem with Individual Letters:
- You’re making it up as you go every time
- Inconsistent = looks unprofessional
- Easy to accidentally overshare
- Time-consuming
- Anxiety-inducing
- POs never know when to expect updates
The Power of a Standardized System:
- Consistent communication = professional credibility
- Clear boundaries = protects clinical relationship
- Predictable timing = reduces PO follow-up emails
- Faster workflow = batch-generate all reports on the 1st
- Less anxiety = you know exactly what to say
Instead of writing individualized letters every month wondering what to say and how much to share, you establish a standardized reporting structure that:
- Gives probation officers exactly what they need (attendance, testing, compliance measures)
- Protects your clinical judgment and therapeutic relationship
- Streamlines your documentation workflow
- Builds professional credibility through consistent communication
- Reduces monthly reporting anxiety
Probation Communication Forms System
Stop staring at blank documents every month. The Probation Communication Forms System includes three standardized forms that give probation exactly what they need while protecting your clinical work.
What’s Inside: Admission Form, Monthly Progress Report, Discharge Summary, plus complete implementation guide for getting PO buy-in.
Sample: Monthly Progress Report Structure
📊 ATTENDANCE & COMPLIANCE
• Sessions attended this month: ___/___
• UA tests completed: ___/___
• Court requirements met: [Checkboxes]
📈 TREATMENT PROGRESS
• Skills development: [Brief description]
• Life stability improvements: [Brief description]
• Treatment engagement level: [Scale]
⚠️ CONCERNS & NEXT STEPS
• Current risk factors: [If any]
• Treatment plan adjustments: [If any]
• Recommendations: [Next steps]
The full system includes all 3 forms plus a step-by-step guide for implementation and PO collaboration.
Getting Buy-In (Which Was Surprisingly Easy)
I scheduled an in-person meeting with probation. Brought my colleague. Brought printed examples of all three forms.
I explained: “I want to make sure I’m giving you what you need in a format that works for you. Does this give you the information you need for your reports?”
They looked at the forms and basically said, “Yeah, sure. This works for us.”
That was it. They were chill about it. Actually seemed to prefer it over the narrative letters.
And honestly? I think I was the only clinician reaching out trying to improve collaboration. Because they seemed almost surprised that someone was proactively trying to make the communication process better.
From 6 Hours to 1.5 Hours Per Month
From that point on, I just filled out the form each month and sent it. Ten minutes max per client. No more agonizing over what to include or leave out. No more avoiding probation communication because it felt overwhelming.
If you have 8 probation clients and were spending 45 minutes per client writing individualized letters:
- Old way: 6 hours per month
- New way: 1.5 hours per month (including setup)
- Time saved: 4.5 hours per month = 54 hours per year
That’s more than a full work week back in your life.
The forms created boundaries that protected both my clinical work AND the therapeutic relationship.
And the best part? Once probation knows they’ll get regular updates from you in a consistent format, they stop reaching out constantly asking for information. Everyone knows what to expect and when to expect it.
How to Implement This System
STEP 1: Customize the Forms (One-Time Setup – 20 minutes)
- Open each Word document
- Replace “[YOUR AGENCY NAME]” with your agency name
- Replace “[YOUR PROGRAM NAME]” with your program name
- Add your logo if desired
- Adjust any checkbox options to fit your program
- Save as your agency’s templates
- Available in multiple formats for maximum flexibility:
- Word documents (.docx) – Fully customizable for your agency
- PDF documents (.pdf) – Ready to print and use immediately
Choose the format that works best for your workflow!
STEP 2: Get Probation Officer Buy-In (Critical!)
Sample Script:
“I want to make sure you’re getting consistent, timely updates on [Client]. I’ve developed a standardized reporting system that I’ll be sending you at admission, monthly during treatment, and at discharge. It includes all the key information you need – attendance, testing results, progress, and any concerns. Would it be helpful if I send you a sample so you can see what to expect?”
Why this works:
- – You’re framing it as serving THEIR needs
- – You’re establishing expectations upfront
- – You’re being proactive about communication
STEP 3: Establish Your Reporting Rhythm
ADMISSION: Send within 48-72 hours of client’s first session
- Shows you’re on top of things
- Sets expectations for ongoing communication
- Establishes your credibility early
MONTHLY: Send by the 5th of each month for previous month
- Consistent timing = you look reliable
- PO knows when to expect updates
- No more “when are you sending that update?” emails
DISCHARGE: Send within 1 week of final session
- Provides closure on the case
- Documents final outcomes
- Maintains your professional relationship for future referrals
STEP 4: Streamline Your Workflow
Create a simple tracking system:
- Calendar reminder on the 1st of each month to generate reports
- Keep a master list of active probation cases
- Batch-generate all monthly reports in one sitting (saves time!)
- Use copy/paste from previous month’s form to speed up process
Pro Tip: On the last day of each month, pull attendance records and have them ready for the 1st so you can knock out all reports quickly.
Probation Communication Forms System
Stop staring at blank documents every month. The Probation Communication Forms System includes three standardized forms that give probation exactly what they need while protecting your clinical work.
What’s Inside: Admission Form, Monthly Progress Report, Discharge Summary, plus complete implementation guide with step-by-step instructions, sample PO buy-in script, what to include vs. what to protect framework, how to handle common situations (missed sessions, positive drug tests, doing well, disagreeing with court mandate), troubleshooting Q&A, and workflow optimization strategies.
👁️ Preview Monthly Report Form ▼
Sample: Monthly Progress Report Structure
📊 ATTENDANCE & COMPLIANCE
- Individual Sessions: Attended ___/___ Missed ___/___
- Group Sessions: Attended ___/___ Missed ___/___
- Drug/Alcohol Testing: Conducted: ___ Results: ___________
- Court requirements met: [Checkboxes for frequency and service types]
📈 TREATMENT PROGRESS (ASAM Dimensions)
- Withdrawal Management: _______________________
- Biomedical Complications: _______________________
- Emotional/Behavioral Issues: _______________________
- Readiness to Change: _______________________
- Relapse Potential: _______________________
- Recovery Environment: _______________________
- Overall Progress: _______________________
📋 SUMMARY
- Progress Since Last Report: ☐ Much Improved ☐ Somewhat Improved ☐ Same ☐ Somewhat Worse ☐ Much Worse
- Tentative Discharge Date: _______________________
- Referrals Made: _______________________
- Upcoming Appointments: _______________________
The complete system includes all 3 professionally designed forms plus an 8-page implementation guide with everything you need to streamline probation communication.
The complete system includes all 3 professionally designed forms plus an 8-page implementation guide with everything you need to streamline probation communication. Would you prefer fillable PDF versions of these forms? Let me know in the comments or email me – I’m always improving these resources based on your feedback!
The Conversations That Keep You Up at Night
- “If I’m honest about my use, will I go to jail?”
- “The judge says I have to quit, but I can’t. What do I do?”
- “Aren’t you supposed to help me stay sober, not tell me how to use drugs?”
These are the questions that freeze counselors. Because there isn’t one “right” answer, and the stakes are massive.
The Difficult Conversations Toolkit I created has word-for-word scripts for these moments—five scenarios with multiple response pathways depending on your client’s situation and your jurisdiction’s requirements.
The Difficult Conversations Toolkit
“If I’m honest, will I go to jail?” The Difficult Conversations Toolkit gives you word-for-word scripts for the five conversations that keep counselors up at night.
What’s Inside: 5 complete conversation scripts with multiple response pathways, documentation guidance, and red flags for each scenario.
Scenario: “If I Tell the Truth, Will I Go to Jail?”
Client says: “I’m scared to tell you what’s really going on. If you tell my PO I’m using, I’ll get violated and go to jail. But I need help.”
OPENING RESPONSE (Always Start Here):
“I’m glad you’re bringing this up, because it’s important we’re both clear about how this works. First, thank you for trusting me enough to even have this conversation. That takes courage, especially knowing your legal situation.”
CLARIFY WHAT YOU’RE REQUIRED TO REPORT:
“Let me be really specific about what I’m required to report based on your court agreement. [Be specific to your jurisdiction]. Here’s what falls under clinical privilege and stays between us: [be specific].”
📝 How to Document: “Client expressed concerns about consequences of disclosing substance use given probation status. Counselor clarified mandated reporting requirements per court agreement and discussed importance of honest communication for effective safety planning.”
The full toolkit includes 5 complete scenarios with multiple response options and red flags.
But here’s the core principle that guides all of them:
Be honest. Be transparent. Create safety.
When a client asks “Will I go to jail if I’m honest?”—don’t lie to them. Don’t minimize the risk. But also don’t shut down the conversation.
“I can’t promise you won’t face consequences. What I can tell you is: getting caught while hiding use usually has worse outcomes than self-reporting and staying engaged in treatment. And whether you decide to disclose right now or not, let’s make sure you’re safe.”
You’re not solving their legal problem. You’re not making false promises. You’re creating a space where they can think through their options and make informed choices.
And you’re making sure they stay alive and engaged in treatment regardless of what they decide to disclose. Speaking of documentation—let me share a system that dramatically reduced my stress around probation communication.
When to Push Back on Court Requirements
Sometimes you need to directly advocate for harm reduction approaches with the court.
For example, when:
- Client would benefit from MAT but court opposes it
- Client is being sanctioned for treatment engagement (testing positive while showing up to all sessions)
- Abstinence-only mandate is creating dangerous conditions
- Court expectations directly conflict with client safety
How to Advocate Effectively for Harm Reduction with Court-Mandated Clients
How: Use data, not philosophy. Frame it around the court’s goals, not yours.
“Research shows MAT reduces overdose deaths by 50% and reduces recidivism by 30% compared to abstinence-only treatment. This approach will help us achieve your goal of reduced recidivism while keeping the client alive.”
The data on MAT in correctional settings is particularly compelling: Rhode Island’s comprehensive MAT program in jails reduced post-release overdose deaths by 60%.
Or: “This client has 100% attendance for the first time in their treatment history. The current approach is working. Escalating consequences now risks disrupting real progress.”
Bring allies—probation officers who understand treatment, other professionals who’ve worked with this client successfully.
And be prepared: sometimes you’ll win. Sometimes you won’t. But you have to try. Whether you’re advocating or simply implementing harm reduction, clarity about your reporting obligations is critical.
Know What You’re Actually Required to Report
Read your court agreement. Seriously. Know exactly what you’re mandated to report.
Typically required:
- New criminal charges
- Client completely disengaging from treatment
- Imminent safety risks
- Whatever your specific agreement mandates
Typically NOT required:
- Every instance of substance use (unless specifically mandated)
- Detailed clinical content beyond basic progress
- Your clinical opinions about what’s “really” happening
Remember, you can often negotiate these requirements upfront.
Many probation officers will agree to graduated reporting frameworks if you propose them during initial treatment planning. But you have to ask. They’re not going to offer it. I know this all sounds complex and maybe overwhelming. So let me show you how it works in real life with an actual client case.
Real-World Example: Harm Reduction with Court-Mandated Clients in Action
Let me show you what this looks like in practice.
Client situation: Marcus, 28, mandated to treatment after third DUI. Court order specifies “complete abstinence from all substances” and weekly UA testing.
Clinical reality: Marcus has severe alcohol use disorder, has never maintained abstinence longer than 3 weeks, and has significant trauma history. Previous abstinence-only treatment resulted in rapid relapse and additional legal charges.
Treatment approach for Harm Reduction with Court-Mandated Clients
- Primary goal (documented): “Client will achieve sustained abstinence from alcohol and demonstrate effective recovery skills”
- Harm reduction strategies (also documented):
- Progressive reduction targets (from daily drinking to weekends only, then to occasions only)
- Safety planning for high-risk situations
- MAT evaluation and referral
- Overdose prevention education
- Regular monitoring and treatment plan adjustments
Month 1: Marcus drinks on weekends but attends all sessions, engages honestly, tests negative during the week.
- Documentation: “Client maintained sobriety 5 days/week, attended 4/4 sessions, actively participated in relapse prevention planning. Weekend use documented; client self-reported and engaged in safety planning and trigger identification. No legal incidents. Treatment plan adjusted to increase weekend support contacts.”
- Court report: “Client demonstrates strong treatment engagement with 100% attendance. Working on relapse prevention skills and protective factor development. Continuing to progress toward treatment goals.”
Month 3: Marcus achieves 3 weeks of complete abstinence, then drinks one evening after job loss. Immediately contacts counselor before using more.
- Documentation: “Client maintained abstinence for 21 consecutive days, demonstrating significant progress. Following job loss stressor, client utilized crisis plan and contacted counselor proactively. Single use episode followed by immediate re-engagement in treatment and safety planning. Client demonstrates strong recovery skills and treatment alliance.”
- Outcome: Court views Marcus as successfully engaged in treatment. Marcus doesn’t face sanctions for honest engagement with recovery process. Clinical relationship remains intact. Marcus eventually achieves sustained abstinence because he learned recovery skills during harm reduction phases rather than cycling through punishment and shame.
This is what “Yes, and” looks like in real life. If you’re feeling uncertain about whether this approach is ethical or effective, let me be clear:
You’re Not Betraying Anyone
The Tension Is Normal
Here’s what I need you to understand:
Harm reduction with court-mandated clients doesn’t betray the court. It fulfills what they actually want: reduced recidivism, client safety, treatment engagement
The research backs this up: harm reduction approaches like LEAD (Law Enforcement Assisted Diversion) reduce recidivism and keep people engaged in treatment longer than punishment-focused models.
You’re Being a Good Clinician
The tension you feel isn’t evidence you’re doing something wrong. It’s evidence you’re thinking critically about how to help your client survive and succeed within a system that doesn’t always make sense.
That tension? That’s you being a good clinician.
Courts want outcomes. Harm reduction with court-mandated clients delivers outcomes. You’re just navigating the space between rigid mandates and human reality—which is exactly what this work requires.
And over time, as you build trust with probation officers, as you demonstrate that you balance clinical support with realistic accountability, as you show results? That tension eases.
Your Clients Will Survive
Not because the system changes. But because you get better at navigating it.
And your clients survive. They progress. They build lives that support recovery—even when that recovery doesn’t look like what the judge ordered at first.
That’s the work of harm reduction with court-mandated clients. And you can do it.
Get the Tools You Need for Harm Reduction with Court-Mandated Clients
This blog barely scratches the surface of navigating court-mandated treatment with harm reduction approaches. To put these strategies into practice, download the four resources designed specifically for this work. Create your free account and you will have access to the following:
Get All 4 Essential Resources
Tools designed specifically for harm reduction with court-mandated clients
Goal Translator
20+ examples of court-friendly harm reduction goals
Progress Note Framework
Document both compliance and clinical reality
Difficult Conversations
Word-for-word scripts for 5 impossible scenarios
Probation Forms System
3 standardized forms that streamline reporting
Each month adds new components to create a comprehensive resource system.
This is the second post in our Justice-Involved Treatment Mastery Series. If you missed the foundation piece “From Compliance to Care: Why Justice-Involved Clients Need a Different Approach,” catch up here before diving into this series.
Next month in the Justice-Involved Treatment Mastery Series: We’ll dive into “Building Therapeutic Alliance in Justice-Involved Treatment”—because none of these strategies work without genuine connection, and mandated treatment creates unique barriers to alliance-building.






