Monthly Strategies for the Underdog Clinician
Featured Highlight: QUARTERLY KITS — YOUR 2026 SURVIVAL SYSTEM
New year, same impossible caseloads. Same documentation pile-up. Same “I should have this figured out by now” spiral.
You made it through December. The holiday sessions. The crisis calls. The clients who relapsed and the ones who white-knuckled it through family dinners. You held space for everyone else’s chaos while managing your own.
Now it’s January, and you’re supposed to feel refreshed. Motivated. Ready to crush your goals.
But you’re tired. And the caseload didn’t shrink just because the calendar flipped.
So we built two kits for exactly this moment:
THE SURVIVAL KIT — FIRST 90 DAYS
For early-career clinicians navigating agency politics, back-to-back sessions, and the constant “am I doing this right?” panic.
What’s Inside:
- Confidence-building frameworks for when imposter syndrome hits
- Agency navigation guides (the unwritten rules nobody tells you)
- Session prep tools for when you have 5 minutes between clients
- Boundary-setting scripts that actually work
- “What they didn’t teach you in grad school” breakdowns
If you’re in your first two years and feel like you’re drowning, this kit was built for you.
THE SIDEKICK KIT — DOCUMENTATION MASTERY
For any experience level struggling with note pile-up, compliance anxiety, and the 60-second session memory gap.
What’s Inside:
- Quick Capture Cards for capturing session details in 60 seconds
- Progress note templates that satisfy compliance AND capture clinical nuance
- The 30-Note Rule framework (don’t learn this the hard way)
- Documentation audit checklists
- Time-blocking strategies for note completion
Whether you’re 3 months in or 13 years deep, if documentation is the thing that keeps you at work late and wakes you up anxious, this kit is for you.
Quarterly Refresh — New Themes Each Season, Available While Supplies Last
Winter 2026 kits drop January 31st. Don’t miss them.
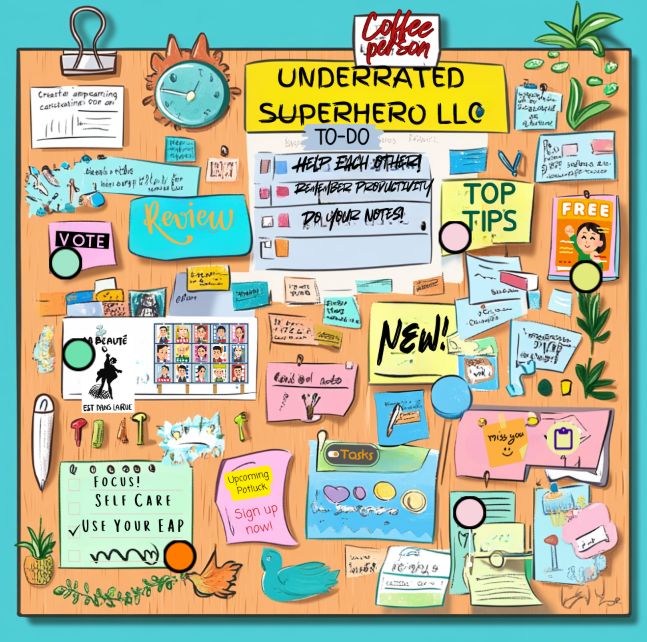
JANUARY MISSION UPDATES
Here’s everything happening this month:
- Featured Board (1/1) – Outpatient Mental Health (OPMH)
- Monthly Content Drop (1/15) – Weekly Pulse Check Worksheet + January Resources
- New Clinician Series (1/4; 1/11; 1/18; 1/25) — Weekly blog posts continuing the series
- Quarterly Kits – Winter 2026 kits drop January 31st
- Justice Involved Mastery Series – 4th Article Release: “Documentation That Satisfies Courts AND Supports Recovery”
Bonus Special: New Clinician Survival Series – Ongoing
Weekly strategies that bridge theory and reality
This month’s releases tackle the unglamorous reality of clinical work: the paperwork that never ends and the creeping feeling that nothing you do actually matters. Real talk for the post-holiday slump.
Recent Posts You May Have Missed:
- “I Can’t Handle This Caseload” – When 40 Clients Feels Like 400
- “My Supervisor Doesn’t Get It” – Navigating Unsupportive Supervision

- “Am I Documenting Wrong?” – Compliance Anxiety and Note Paranoia
- “They Keep Relapsing” – When Client Progress Isn’t Linear

- “I Don’t Know Enough” – When Knowledge Gaps Feel Dangerous
Coming in January:
- “Nobody Told Me About the Paperwork” — When the administrative burden feels heavier than the clinical work
- “I’m Not Making a Difference” — When you’ve been doing this long enough to wonder if it matters
What Makes This Series Different:
Unlike generic “new professional” advice, this series specifically addresses the unique challenges of behavioral health work. Each post includes the uncomfortable thought, why it happens, what to do about it, and tools you can use immediately—decision trees, scripts, and reflection prompts.
Research indicates that up to 82% of healthcare professionals experience imposter syndrome at some point in their careers. These posts don’t just acknowledge that—they give you practical strategies for working through it.
Follow along: New posts drop every Sunday.
IMPLEMENTATION NOTES
January’s series tackles the unglamorous reality of clinical work: the paperwork that never ends and the creeping feeling that nothing you do actually matters.
The post-holiday slump is real. Your clients are struggling with broken resolutions and the gap between where they wanted to be by now and where they actually are. And honestly? You might be feeling the same thing.
These posts meet you there — no toxic positivity, no “new year new you” nonsense. Just honest strategies for getting through the hard parts.
FEATURED BOARD: OUTPATIENT SETTINGS
Outpatient work is a different beast.
You see clients for 45 minutes once a week — maybe twice if you’re lucky — and somehow you’re supposed to create lasting change. They walk out your door and back into the same environments, relationships, and stressors that brought them to you in the first place.
You don’t have the controlled environment of residential. You don’t have daily check-ins. You don’t have a treatment team watching them 24/7.
You have one hour. Maybe less after they show up late and you have to end on time for your next client.
This interactive board provides frameworks, tools, and strategies specifically designed for outpatient settings — where every minute counts and continuity of care is a constant challenge.
What It Covers:
- Maximizing Limited Session Time — How to structure 45-minute sessions for maximum impact when you’re addressing multiple concerns
- Between-Session Engagement — Tools and strategies for maintaining momentum when you only see clients weekly
- Crisis Management in Outpatient Settings — When to refer up, when to hold, and how to document your decision-making
- Coordination with Prescribers — Communication templates and collaboration frameworks
- Managing No-Shows and Late Cancellations — Policies, scripts, and strategies that actually work
- Treatment Planning for Outpatient — Goals and objectives that make sense for limited-contact treatment
- Discharge Planning — Knowing when someone’s ready and how to transition them out successfully
Perfect For:
- ✓ Community mental health clinicians
- ✓ Private practice therapists
- ✓ Outpatient SUD counselors
- ✓ Clinicians transitioning from residential to outpatient settings
- ✓ Anyone feeling like 45 minutes isn’t enough time
QUICK WIN TOOL OF THE MONTH
THE WEEKLY PULSE CHECK
FIND THEM NOW IN YOUR PROFESSIONAL RESOURCES
Five questions. Every Friday. Two minutes.
That’s it. No elaborate self-care routine. No 10-step reflection journal. No app that sends you 47 notifications about mindfulness.
Just a quick gut-check before you leave for the weekend.
The 5 Questions:
- How many notes am I behind? (Be honest. The number matters less than knowing the number.)
- Did I take lunch at least 3 days this week? (Not eating at your desk while charting. Actual lunch.)
- What’s one thing I did well this week? (One clinical win. One good session. One moment you handled well.)
- What’s one client situation I need consultation on? (The one you’re carrying. The one keeping you up. Name it.)
- What do I need this weekend to recover? (Sleep? Solitude? Social time? Movement? What does your body actually need?)
Why This Works:
Most clinicians don’t process their week until they’re lying in bed Sunday night dreading Monday. By then, everything feels heavy and vague — a general sense of overwhelm without specifics.
The Weekly Pulse Check forces you to NAME things before you leave on Friday. And what gets named gets managed.
How to Use It:
- End of day Friday: Take 2 minutes before you log off. Answer the 5 questions — out loud, on paper, in a notes app, doesn’t matter.
- In supervision: Bring your answers. It’s a built-in agenda.
- With a colleague: Do it together. Friday accountability check-in.
The goal isn’t perfection. The goal is awareness. You can’t fix what you won’t look at.
UNDERRATED TACTIC: THE “WHAT IF” PRE-FRAME
STOP WAITING FOR SUPERVISION TO PROCESS
Most clinicians carry the week’s stress home because they never stop to ask themselves what’s actually weighing on them.
You finish your last session. You chart (or don’t). You grab your stuff and leave. And somewhere on the drive home, the weight settles in — but you can’t name it. It’s just… heavy. Vague. A general sense that this week was hard and next week will be too.
By Sunday night, you’re dreading Monday but you couldn’t tell someone exactly why.
The Problem:
You’re waiting for supervision to process. Or therapy. Or a breakdown. Instead of checking in with yourself regularly, you let everything accumulate until it spills over.
The Fix:
Before you leave on Friday, answer the 5 Pulse Check questions. Out loud or on paper — doesn’t matter. What matters is you NAME it before you carry it home.
The client you’re dreading? Name it.
The note pile that’s growing? Name it.
The win you forgot to celebrate? Name it.
The consultation you’ve been putting off? Name it.
What gets named gets managed. What stays vague stays heavy.
Why Friday?
Because weekends are supposed to be recovery time. But they can’t be if you’re carrying unnamed stress into them. The Friday 5 creates a boundary between work-week and weekend — a moment where you consciously set things down instead of unconsciously dragging them home.
The Ripple Effect:
When you name what’s weighing on you, you can actually DO something about it:
- That client you’re dreading? Bring it to supervision Monday.
- The note pile? Block 30 minutes Monday morning to chip away at it.
- The win you forgot? Actually let yourself feel good about it.
- The consultation you need? Email a colleague this weekend.
You’re not solving everything Friday at 5pm. You’re just naming it so it doesn’t follow you home unnamed.
PAIRS PERFECTLY WITH THIS MONTH’S QUICK WIN: THE WEEKLY PULSE CHECK
Use the worksheet to structure your Friday check-in. Keep it in your desk, your bag, or your notes app. Make it a ritual.
Two minutes. Five questions. Every Friday.
JUSTICE-INVOLVED TREATMENT MASTERY SERIES
Month 4: “Documentation That Satisfies Courts AND Supports Recovery”
Releasing January 11th
You’re caught between two systems with different definitions of success.
The court wants compliance. Attendance. Clean UAs. Check boxes that prove your client is “doing the work.”
Clinical best practice wants progress. Engagement. Harm reduction. Nuanced documentation that captures the messy, non-linear reality of recovery.
And you’re stuck in the middle, trying to write notes that satisfy both — often feeling like you’re failing at least one of them.
This month’s Mastery Series article tackles the documentation dilemma head-on:
What’s Inside:
- The Yes-And Progress Note Framework — How to document court compliance AND clinical progress in the same note
- Treatment Plan Templates for Justice Settings — Goals and objectives that satisfy legal requirements without abandoning clinical integrity
- Language That Works in Both Systems — Specific phrasing that courts accept and clinicians can stand behind
- What NOT to Document — The notes that will come back to haunt you (and your client)
- Progress Note Examples — Real examples of court-compliant notes that don’t sacrifice clinical nuance
Plus Subscriber-Exclusive Resources:
→ Treatment Plan Templates for Justice Settings
→ Progress Note Examples – Court Compliant
→ Dual Accountability Documentation System
Based on our comprehensive Justice-Involved Interactive Board
Ultimately, remember that you don’t have to reinvent the wheel. Explore The Underrated Superhero Resource Hub for ready-to-use tools, templates, and strategies that save you prep time and keep you focused on care.
– The Underrated Superhero
Prefer to download and read later?